MEMS® bottle use among adolescents/emerging adults with SCD

[ad_1]
Introduction
Due to advancements in uncovering the mechanisms underlying sickle cell disease (SCD), the landscape of SCD treatment is rapidly evolving.1 Three new medications have been approved for this population in recent years, with 28 potential therapies currently under investigation.1 However, the ultimate impact of these therapies on health outcomes will depend on patient adherence. Adolescents and emerging adults (ie, teens through the early twenties)2 with SCD are at particular risk for suboptimal adherence,3,4 contributing to increased rates of disease complications and early death during this period.5,6 Identifying accurate, acceptable, and feasible adherence assessment methods for adolescents and emerging adults with SCD is critical for treatment effectiveness research and clinical care.
Electronic adherence monitoring devices (EAMDs) are medication bottles with built-in technology that records date- and time-stamps of device openings and are considered a gold standard for adherence assessment across many pediatric populations.7 However, little is known about their feasibility among individuals with SCD. Berkovitch et al8 documented significant challenges using Medication Event Monitoring System (MEMS®) bottles for young children with SCD (<7 years) due to technological difficulties (eg, bottles breaking after being dropped or liquid formulation penetrating the device). A recent study using an alternative EAMD (ie, GlowCap) reported similar issues with equipment malfunctioning among youth with SCD ages 2–21 years.9 Conversely, among a small sample of SCD patients ages 7–18 years, use of MEMS® was described as a highly practical method of assessing adherence over the course of one year.10 While these studies offer useful preliminary data on the feasibility of EAMDs in pediatric SCD, they were conducted in samples with broad age ranges and did not explore unique barriers and facilitators during adolescence and emerging adulthood.
To address this gap, this study sought to examine MEMS® bottle use among adolescents and emerging adults with SCD (ages 13–21 years) to: 1) evaluate the feasibility of MEMS® bottle use, defined by the percentage of participants that initiated MEMS® bottle use, continued to use the bottle over the study period, and returned the bottle at study visits for data download; and 2) explore barriers and facilitators to MEMS® bottle use. Based on existing retention guidelines for observational prospective studies and randomized trials,11,12 we defined cut-points for feasibility as follows: 100% of participants who enrolled in the study would initiate MEMS®, >80% would use MEMS® through the final study endpoint, and >60% would return the bottle within two weeks of scheduled study visits. We expected that adolescents and emerging adults with SCD would report modifiable barriers and facilitators to MEMS® use.
Materials and Methods
As part of a larger study of a self-management intervention,13 participants were asked to use a MEMS® bottle to store and administer their daily oral medication (ie, hydroxyurea or deferasirox) for the 18-week (126 days) study duration. The larger study included baseline (day 1), post-treatment (day 42), and follow-up assessments (day 126). Participants were instructed to provide their MEMS® bottle for data download at the post-treatment and follow-up assessment visits. A survey assessing barriers to and facilitators of MEMS® use was administered at both post-treatment and follow-up. Participants were compensated $20 at post-treatment and $20 at follow-up if they returned the MEMS® bottle for data download. Study procedures were approved by the local institutional review board. This study complies with the Declaration of Helsinki.
Study participants were English-speaking individuals diagnosed with SCD who were between the ages of 13 and 21 years and had an active prescription for hydroxyurea or deferasirox at the time of study enrollment. Exclusion criteria included presence of a neurocognitive disability based on medical record review. All eligible adolescents and emerging adults received a letter and flyer in the mail followed by a phone call to explain the study. Patients were also recruited during clinic visits and hospitalizations. Of the 19 patients approached, 18 (94.7%) agreed to participate and enrolled in the study. Informed consent was obtained from a parent or legal guardian for patients under 18 years of age and from adult patients ages 18+ years; assent was obtained from teens ages 13–17 years.
Participant demographic characteristics were assessed via a self-report (for participants ages 18+ years) or parent-report questionnaire (for participants ages 13–17 years). MEMS® 6th generation TrackCap bottles (AARDEX Group, Boulder, CO) were used for electronic adherence monitoring. MEMS® bottles have an embedded computer chip that digitally records when they are opened. Data obtained from MEMS® bottles were downloaded when the participants returned the bottles at post-treatment and follow-up assessments. Two open-ended survey questions developed by our team based on prior research were used to assess participant self-reported barriers (eg, reasons for missing doses) and facilitators (eg, strategies such as alarms and reminders) to MEMS® use: “What are some reasons you might have missed a dose of your medicine?” and “What types of things help you to remember to take the medicine?”.
Descriptive statistics were calculated to assess MEMS® bottle feasibility, defined as initiation (ie, percentage of those enrolled that initiated MEMS® use), sustained use (ie, percentage of participants that continued to open the MEMS® bottle at least once per week over the study period), and bottle provision at study visits (ie, percentage of participants that returned MEMS® bottles for data download ±2 weeks of scheduled study visit = “on time”). While not the primary focus of this study, we also calculated adherence rates based on data recorded via MEMS®. Specifically, the number of days that the MEMS bottle was opened was divided by the total number of study days (ie, 126) for each participant; descriptive statistics were then calculated to examine adherence rate for the sample. Open-ended survey responses regarding barriers and facilitators to MEMS® use were reviewed and summarized.
Results
Eighteen non-Hispanic Black/African American adolescents and emerging adults (n = 11 male; M = 17.8 years old, SD = 2.6) with SCD (n = 18 HbSS) were enrolled in the study and asked to use a MEMS® bottle to store and administer their hydroxyurea (n = 14) or deferasirox (n = 4). On average, participants started taking their medication 4.4 years prior to enrolling in the study (Range = 0–10, SD = 3.8). Half of the sample (n = 9) reported annual family income of ≤ $10,000, n = 2 reported $13,000–$20,000, and n = 3 reported $30,000–$50,000; n = 4 did not provide data on income. Regarding health insurance, most participants (n = 10) had public insurance, n = 4 had private insurance, and n = 3 had a combination of public and private insurance coverage.
All 18 participants (100%) initiated MEMS® use and 11 (61.1%) sustained MEMS® use through the final study endpoint. Eight (44.4%) and 2 (11.1%) participants provided their MEMS® bottle for download “on time” at post-treatment (42 days) and follow-up (126 days), respectively. Participants took a median of 26.2% of doses across the 126 days (SD = 22.4; Range=0.79%–79.3%; see Figure 1). Barriers to MEMS® bottle use included medication changes (ie, medication holds due to labs [n = 2, 11.1%], dose changes due to weight loss/gain [n = 1, 5.6%]), running out of medication (n = 3, 16.7%), forgetting to take medication (n = 4, 22.2%), and transitioning from pediatric to adult care (n = 1, 5.6%). Facilitators included setting a timer (n = 1, 5.6%), tip sheets (eg, places to store the MEMS® bottle; n = 1, 5.6%), reminders to place refills in bottle (n = 1, 5.6%), mobile apps (n = 1, 5.6%), and reminder calls (n = 1, 5.6%).
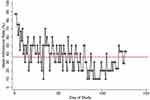 |
Figure 1 Daily adherence rates. Note: Red line indicates overall mean adherence across the study period. |
Discussion
As SCD management increasingly includes self-administration of oral medications, adherence assessment has become a critical component of research on medication effectiveness and clinical care. Our findings suggest that while adolescents and emerging adults with SCD appear receptive to initiating electronic adherence monitoring via MEMS®, ensuring sustained use and timely provision of bottles for data download will likely require additional supports. For example, EAMDs that automatically transmit data in real-time via Bluetooth or cellular connections would eliminate the need for patients to bring bottles to study visits for data downloads. With remote monitoring capabilities, researchers could conduct intermittent data downloads to track and address equipment malfunctioning and user error, thereby enhancing the completeness and accuracy of data obtained.7 These features may be particularly important for adolescents and emerging adults with SCD, who often experience social determinants of health barriers that can impact adherence monitoring (eg, transportation barriers, economic instability, lapses in health insurance coverage).
Other features offered by some electronic monitoring devices (eg, alarms, text message reminders, adherence calendars, caregiver notification, refill due notice)7,14 may also help to minimize barriers reported by adolescents and emerging adults with SCD in this study. Prior research suggests that for adolescents and young adults with SCD, daily medication reminders and medication logs are among the most preferred features of technology-based adherence interventions.15 Support strategies should be tailored to an individual’s unique barriers to yield the greatest impact. However, it should be noted that features that go beyond passive monitoring can influence medication adherence behavior and may not be appropriate for all studies (eg, observational designs and run-in, baseline, and post-treatment phases of intervention trials).7 Regardless of the specific EAMD features enabled, it is recommended that researchers conduct pilot testing to identify and proactively address equipment issues as well as carefully educate patient, healthcare provider, and study staff on appropriate device use to enhance data quality.
Several limitations should be noted. Consistent with prior pilot studies and research using EAMDs in pediatric SCD, sample size for this study was small. Moreover, we did not administer other adherence assessments (eg, self-report, prescription refill data) or examine associations between adherence and demographic and clinical characteristics. Larger studies are needed to evaluate concordance between rates of adherence obtained via EAMDs and other assessments and to validate electronically monitored medication adherence with relevant clinical outcomes. In addition, data on barriers to and facilitators of MEMS® bottle use were limited in that they were drawn from open-ended responses to investigator-developed survey items; future studies should consider conducting interviews and formal qualitative analysis of factors influencing feasibility of electronic adherence monitoring within this population. Future research should also consider screening for social determinants of health and exploring how these impact electronic adherence monitoring.
Conclusion
This study suggests that MEMS® bottles are potentially feasible for tracking adherence to oral medications among adolescents and emerging adults with SCD. Electronic monitoring devices are not a solution to medication adherence, but rather, one component of an adherence support strategy. Given the rapid development of additional treatment options for individuals with SCD, identifying accurate, acceptable, and feasible adherence assessments for this population is a high research and clinical priority for the field.
Abbreviations
EAMDs, electronic adherence monitoring devices; MEMS®, Medication Event Monitoring System; SCD, sickle cell disease.
Data Sharing Statement
De-identified data are available upon reasonable request.
Ethics Approval and Informed Consent
This study was approved by the Cincinnati Children’s Hospital Medical Center institutional review board. Informed consent/assent was obtained from all participants included in this study.
Acknowledgments
We thank the youth with SCD who participated in this study as well as the study coordinators.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all of these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was supported by the National Heart, Lung, and Blood Institute at the National Institutes of Health [K07HL108720] and a Cincinnati Children’s Hospital Medical Center Place Outcomes Award (LEC). The content of this paper is solely the responsibility of the authors and does not necessarily represent the views of the National Institutes of Health or Cincinnati Children’s Hospital Medical Center.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Ballas SK. The evolving pharmacotherapeutic landscape for the treatment of sickle cell disease. Mediterr J Hematol Infect Dis. 2020;12(1):e2020010. doi:10.4084/mjhid.2020.010
2. Arnett JJ. Adolescence and Emerging Adulthood: A Cultural Approach.
3. Walsh KE, Cutrona SL, Kavanagh PL, et al. Medication adherence among pediatric patients with sickle cell disease: a systematic review. Pediatrics. 2014;134(6):1175–1183. doi:10.1542/peds.2014-0177
4. Loiselle K, Lee JL, Szulczewski L, Drake S, Crosby LE, Pai AL. Systematic and meta-analytic review: medication adherence among pediatric patients with sickle cell disease. J Pediatr Psychol. 2015;41(4):406–418. doi:10.1093/jpepsy/jsv084
5. Quinn CT, Rogers ZR, McCavit TL, Buchanan GR. Improved survival of children and adolescents with sickle cell disease. Blood. 2010;115(17):3447–3452. doi:10.1182/blood-2009-07-233700
6. Hamideh D, Alvarez O. Sickle cell disease related mortality in the United States (1999–2009). Pediatr Blood Cancer. 2013;60(9):1482–1486. doi:10.1002/pbc.24557
7. McGrady ME, Ramsey RR. Using electronic monitoring devices to assess medication adherence: a research methods framework. J Gen Intern Med. 2020;35(9):2707–2714. doi:10.1007/s11606-020-05905-z
8. Berkovitch M, Papadouris D, Shaw D, Onuaha N, Dias C, Olivieri NF. Trying to improve compliance with prophylactic penicillin therapy in children with sickle cell disease. Br J Clin Pharmacol. 1998;45(6):605–607. doi:10.1046/j.1365-2125.1998.00730.x
9. Inoue S, Kodjebacheva G, Scherrer T, et al. Adherence to hydroxyurea medication by children with sickle cell disease (SCD) using an electronic device: a feasibility study. Int J Hematol. 2016;104(2):200–207. doi:10.1007/s12185-016-2027-x
10. Olivieri NF, Vichinsky EP. Hydroxyurea in children with sickle cell disease: impact on splenic function and compliance with therapy. J Pediatr Hematol Oncol. 1998;20(1):26–31. doi:10.1097/00043426-199801000-00004
11. Kristman V, Manno M, Côté P. Loss to follow-up in cohort studies: how much is too much? Eur J Epidemiol. 2004;19(8):751–760. doi:10.1023/B:EJEP.0000036568.02655.f8
12. Fewtrell MS, Kennedy K, Singhal A, et al. How much loss to follow-up is acceptable in long-term randomised trials and prospective studies? Arch Dis Child. 2008;93(6):458–461. doi:10.1136/adc.2007.127316
13. Crosby LE, Joffe NE, Peugh J, Ware RE, Britto MT. Pilot of the chronic disease self-management program for adolescents and young adults with sickle cell disease. J Adolesc Health. 2017;60(1):120–123. doi:10.1016/j.jadohealth.2016.08.022
14. McGrady ME, Holbein CE, Smith AW, et al. An independent evaluation of the accuracy and usability of electronic adherence monitoring devices. Ann Intern Med. 2018;169(6):419–422. doi:10.7326/M17-3306
15. Badawy SM, Thompson AA, Liem RI. Technology access and smartphone app preferences for medication adherence in adolescents and young adults with sickle cell disease. Pediatr Blood Cancer. 2016;63(5):848–852. doi:10.1002/pbc.25905
[ad_2]
Source link
