KFF/The Undefeated Survey on Race and Health – Main Findings – 9557

[ad_1]
Introduction
Racial disparities in health and health care have been longstanding and persistent in the United States. Even before the coronavirus pandemic, African Americans were experiencing lower rates of health insurance coverage, increased barriers to accessing health care, and worse health outcomes compared to their White counterparts. Black adults in the U.S. also face social and economic inequities, including higher rates of unemployment, that play a major role in shaping health. Beyond these factors, research shows that historic abuse and mistreatment of communities of color by the medical system and ongoing racism and discrimination drive disparities in health, contributing to lower quality of care, distrust of the health care system, and stress and trauma. Reflecting these experiences, KFF surveys dating back to 1999 have documented a gap in trust of health care providers between Black and White Americans.
The COVID-19 pandemic has drawn new attention to and compounded these existing disparities in health and health care. Since the pandemic hit the U.S. in early 2020, a growing body of research has consistently shown that people of color have borne a disproportionate burden of COVID-19, including being at increased risk for exposure and experiencing higher rates of infection, hospitalization, and death. Data also show that people of color are taking a harder hit financially from the economic downturn associated with the pandemic, experiencing higher rates of increases in unemployment and difficulty paying for basic needs. In addition, the deaths of Black men and women including George Floyd and Breonna Taylor at the hands of police, and ensuing protests around the country and the world, have shined a spotlight on inequities in the criminal justice system, and the threat of violence that feels like an all-too-common occurrence for many Black Americans.
In light of these facts, KFF partnered with ESPN’s The Undefeated to conduct a survey exploring African Americans’ views and experiences of being Black in America, focusing on experiences with racism and discrimination, including within the health care system; the impacts of the pandemic; and views of a potential coronavirus vaccine. The survey of over 1,700 U.S. adults includes an oversample of nearly 800 Black Americans to allow for in-depth reporting among this group by age, gender, education, and income, as well as comparison groups of White and Hispanic adults. Other groups, including Asian, American Indian and Alaska Native, and Native Hawaiian and Pacific Islander people are included in the total in proportion to their population, but the sample size is not sufficient to break their responses out separately.
This work builds on KFF’s long history of documenting racial and ethnic disparities in health and health care, as well as our history of using surveys to document the views and experiences of African Americans on broader issues of race, culture, and discrimination in partnership with media organizations like CNN and The Washington Post.
Executive Summary
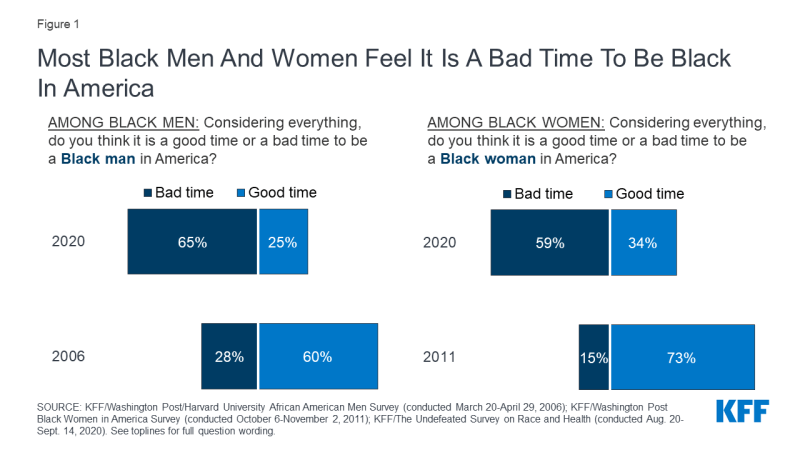
- The share of Black adults who believe it is a good time to be Black in America has plummeted in recent years, but most believe the current protest movement will lead to meaningful change that will improve Black people’s lives. Just a quarter of Black men now say it is a good time to be a Black man in America, down from 60% in 2006, and just a third of Black women (34%) now say it’s a good time to be a Black woman, down from 73% in 2011. Yet almost six in ten Black adults (57%) believe the current protest movement and fight for racial equality will lead to meaningful change that will improve the lives of Black people in the United States.
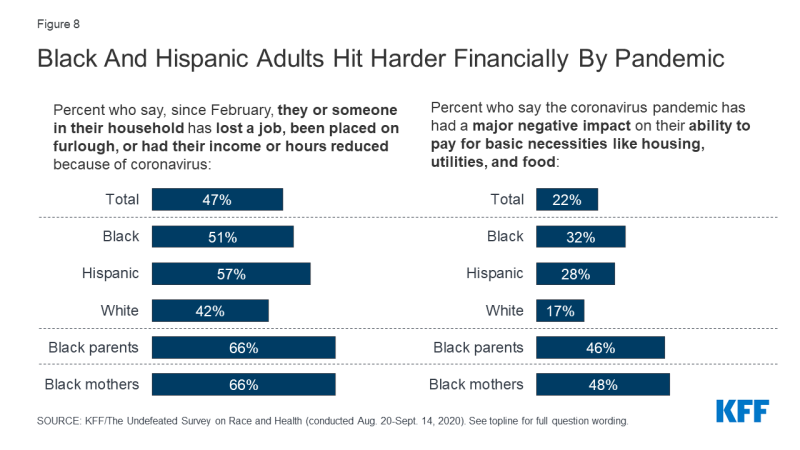
- Black Americans – and Black parents in particular – have been especially hard-hit by the coronavirus pandemic, both financially and emotionally. Half of Black adults (compared to 42% of White adults) say someone in their household has lost a job or had their income reduced as a result of the pandemic, and one-third (compared to 17% of White adults) say it has had a major negative impact on their ability to afford basic needs like housing, utilities, and food. Among Black parents, the share reporting income loss rises to two-thirds, and almost half (46%) of Black parents report a major problem affording necessities. Black parents are also more likely than White parents to say the pandemic has had a major impact on their relationships with family members and their ability to care for their children. Overall, Black adults are more likely than their White counterparts to say they that know someone who has died from COVID-19, that they are worried about contracting the virus at work, and that the pandemic has caused a major decline in their mental health. Two-thirds of Black adults think that the federal government would be taking stronger action to fight the pandemic if White people were getting sick and dying at higher rates than people of color.
- About half of Black adults say they would not want to get a coronavirus vaccine if it was deemed safe by scientists and freely available, with safety concerns and distrust cited as the top reasons. By contrast, most White adults say they would get vaccinated, and those who wouldn’t get a vaccine are more likely to say they don’t think they need it. Majorities of Black adults also lack confidence that the vaccine development process is taking the needs of Black people into account, and that when a vaccine becomes available it will have been properly tested and will be distributed fairly.
- Seven in ten Black adults believe race-based discrimination in health care happens at least somewhat often, and one in five say they have personally experienced it in the past year. Black adults are also more likely than those who are White to report some specific negative experiences with health care providers, including providers not believing they were telling the truth or refusing to provide pain medication or other treatments they thought they needed. Two-thirds of Black adults – across income and education levels – say it is difficult to find a health care provider who shares their background and experiences, and one-quarter say they have never received care from a Black doctor. Reflecting these experiences, Black adults are less likely than their White counterparts to say they trust doctors, local hospitals, and the health care system to do what is right for their communities.
- Black women – particularly mothers – report experiencing even higher rates of discrimination in health care settings. Among Black women who have a child under the age of 18, 37% say they have been treated unfairly based on their race while getting health care for themselves or a family member in the past year, and 41% say there was a time in the past three years when a health care provider talked down to them or didn’t treat them with respect. (Among Black men these shares are 15% and 17%, respectively). Black women overall are also more likely than Black men to report feeling that a health care provider didn’t believe they were telling the truth, assumed something without asking, or suggested they were personally to blame for their health problems.
The Big Picture: Being Black in America Today
Majorities of Black men and women, regardless of age, income, and education, say it is a bad time to be Black in America. The survey finds that Black men and women largely agree that it is a difficult time to be Black in America, a finding that is perhaps not surprising given the disproportionate impact of the coronavirus pandemic on Black families and the national attention drawn to police violence against Black Americans, along with broader issues of systemic racism, over the summer of 2020. Among Black men, just one quarter say now is a good time to be a Black man in America, down 35 percentage points from 60% in a 2006 survey conducted by KFF and The Washington Post. Similarly, the share of Black women who say it’s a good time to be a Black woman in America dropped by more than half, from 73% in a 2011 KFF/Washington Post survey to 34% in 2020. Now, majorities of both groups say it is a bad time to be a Black man (65%) or a Black woman (59%), a finding that holds true across Black men and women regardless of age, income, and education.
When asked to say in their own words the biggest concerns facing them and their families right now, 36% of Black adults cite financial issues and a similar share (34%) cite concerns related to the COVID-19 pandemic. These are also the top two concerns mentioned by White and Hispanic adults, though Black adults are 10 percentage points more likely than White adults to name financial challenges among their top concerns (36% vs. 26%). Conversely, White adults are more likely than Black or Hispanic adults to cite concerns about government and politics, such as the upcoming presidential election (15% of White vs. 7% of Black and 5% of Hispanic). Notably, six percent of Black adults cite issues related to racism as being among their top concerns, and three percent cite worries about police violence.
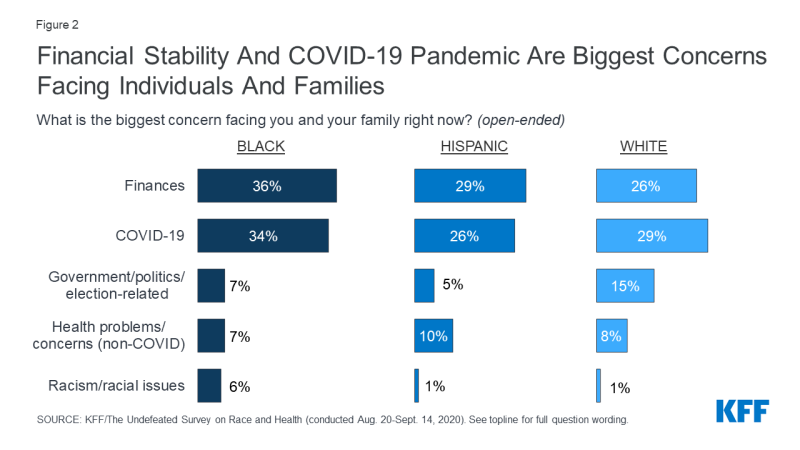
Figure 2: Financial Stability And COVID-19 Pandemic Are Biggest Concerns Facing Individuals And Families
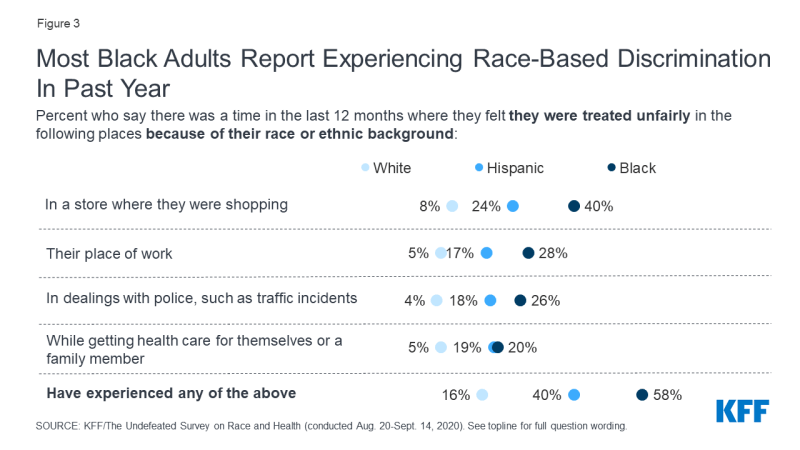
Most Black adults report experiencing race-based discrimination in the past year. The survey finds that nearly six in ten (58%) Black adults say they were treated unfairly while shopping, working, getting health care, or interacting with police in the past 12 months because of their race or ethnic background. Four in ten Hispanic adults also report experiencing such unfair treatment, compared with just 16% of White adults.
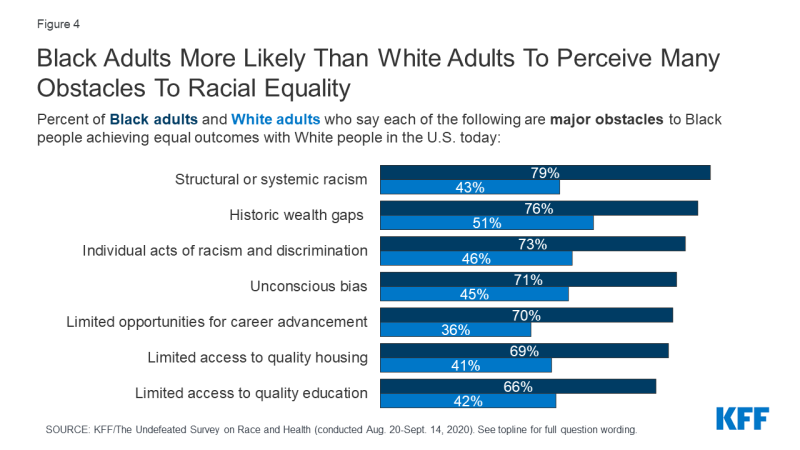
Black adults identify multiple structural and systemic barriers as major obstacles to achieving equal outcomes with White people, as well as individual acts of racism and unconscious bias. When asked about obstacles to Black people achieving equal outcomes with White people in the U.S., larger shares of Black adults compared to White adults view various things as “major obstacles.” At least three-quarters of Black adults see structural or systemic racism (79%) and historic wealth gaps (76%) as major barriers, and about seven in ten say the same about individual acts of racism and discrimination (73%), unconscious bias (71%), limited opportunities for career advancement (70%), and limited access to quality housing (69%). Two-thirds of Black adults see limited access to quality education as a “major obstacle.” The share of White adults viewing each of these things as a major obstacle to Black people achieving equal outcomes with White people is at least 20 percentage points lower than the share of Black adults giving the same answer.
Most Black adults report that unconscious bias, racism and discrimination, and structural and system barriers have been personal obstacles in their lives. When Black adults were asked whether this same list of items had been an obstacle in their own life, the list was similar, but unconscious bias was at the top (71% say this has been an obstacle), followed by about two-thirds who named individual acts of racism and discrimination (65%), structural or systemic racism (65%), and historic wealth gaps (63%). Nearly as many (57%) say that limited opportunities for career advancement has been a personal barrier. Fewer Black adults – about four in ten – see limited access to quality housing (44%) or quality education (41%) as obstacles in their own lives.

Figure 5: Most Black Adults Say Unconscious Bias, Discrimination, And Systemic Racism Have Been Personal Obstacles
Although unconscious bias ranks at the top of the list of personal obstacles, most Black adults who report experiencing discrimination in the past 12 months (58% of all Black adults) say that when people treat them unfairly based on their race, they are usually discriminating on purpose (70%), rather than being unaware they are being unfair (27%).
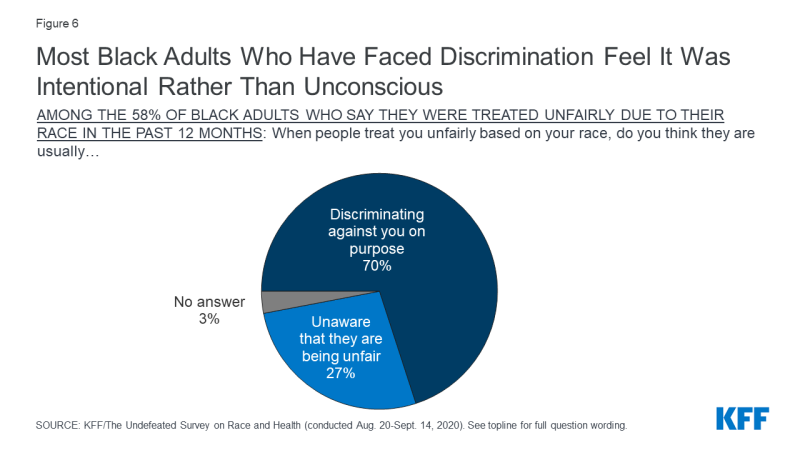
Figure 6: Most Black Adults Who Have Faced Discrimination Feel It Was Intentional Rather Than Unconscious
Despite these challenges, Black Americans are not without hope, with most believing the current protest movement will lead to meaningful change that will improve their lives. A majority (57%) of Black adults say they believe that “the current protest movement and fight for racial equality will lead to meaningful change that will improve the lives of Black people,” while a slight majority (53%) of White adults say they do not think the movement will lead to meaningful change. Hispanic adults respond similarly to Black adults, with 56% saying protests will lead to meaningful change. These racial differences at least partially reflect differing partisanship; 72% of Democrats (including 65% of Black Democrats and 75% of white Democrats) expect the protest movement to lead to meaningful change, while eight in ten Republicans (the large majority of whom are White) expect no meaningful change.
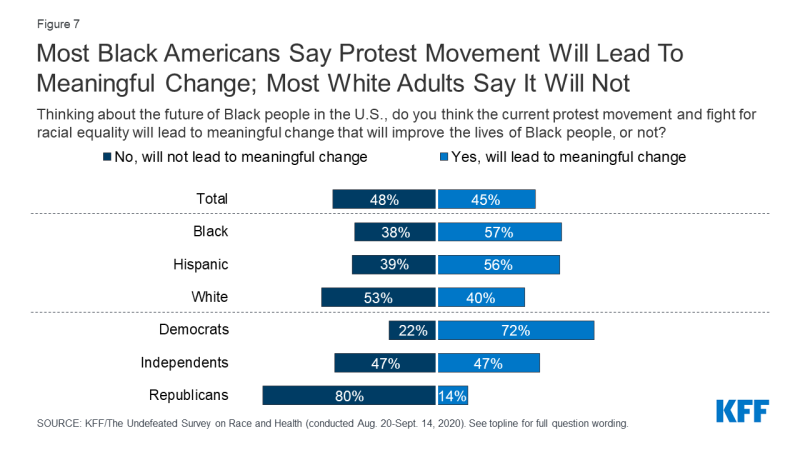
Figure 7: Most Black Americans Say Protest Movement Will Lead To Meaningful Change; Most White Adults Say It Will Not
The Disproportionate Impact of the COVID-19 Pandemic
Beyond its stark impacts on health and mortality, the coronavirus pandemic is also having significant economic impacts and taking a toll on individuals’ mental and emotional health. Similar to the disproportionate rates of infection, serious illness, and death people of color are experiencing from the virus, the survey findings show that they also are bearing a disproportionate burden of negative consequences on their financial and emotional well-being.
Black and Hispanic adults are more likely to report employment disruptions and financial hardships associated with the pandemic compared to their White counterparts. With unemployment rising to record levels, about half of all U.S. adults, including higher shares of those who are Black (51%) or Hispanic (57%) compared to 42% of White adults, say that they or someone in their household has lost a job, been placed on furlough, or had their hours or income reduced as a result of the pandemic. The shares are even higher among Black parents with children under age 18 living at home, two-thirds (66%) of whom report a pandemic-related disruption in employment or income.
For many, these employment disruptions are leading to significant financial struggles. About three in ten of those who are Black (32%) or Hispanic (28%) say the pandemic has had a “major negative impact” on their ability to pay for basic necessities like housing, utilities, and food, compared with 17% of White adults. Again, Black parents have been hit particularly hard, with nearly half (46% of Black parents overall, 48% of Black mothers) saying the pandemic has had a major negative impact on their ability to pay the bills.
Black parents also report disproportionate impacts on their ability to care for their children and their family relationships. Larger shares of Black parents than White parents say the coronavirus pandemic has had a “major negative impact” on their ability to care for their children (32% vs. 13%) and on their relationships with family members (25% vs. 12%). Majorities of both Black parents (60%) and White parents (59%) say the pandemic has had a major negative impact on their children’s education.
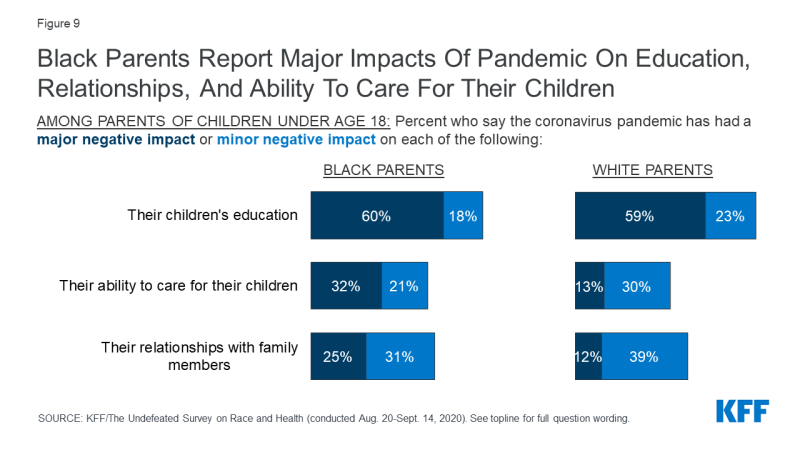
Figure 9: Black Parents Report Major Impacts Of Pandemic On Education, Relationships, And Ability To Care For Their Children
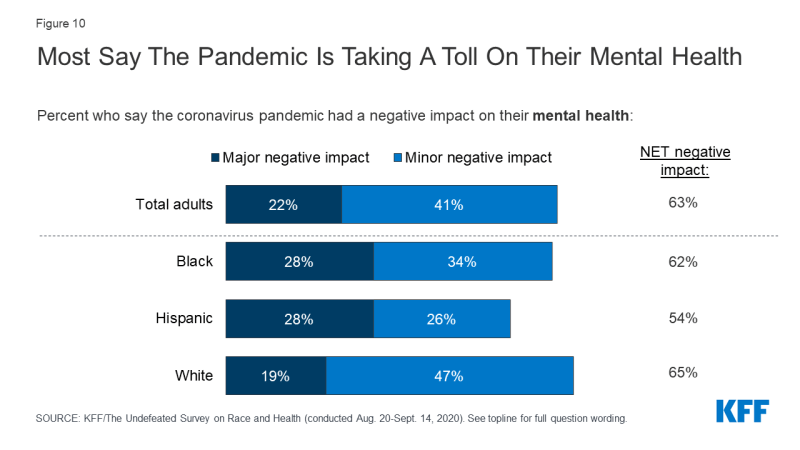
Black and Hispanic adults are more likely to report the pandemic has had a major negative impact on their mental health and to say they know someone who has died from coronavirus compared to those who are White. The coronavirus pandemic is taking an emotional toll on many Americans, including people of color. While more than half of adults across racial and ethnic groups say the pandemic has had a negative impact on their mental health, the share saying it has had a “major negative impact” is higher among Black and Hispanic adults (28% each) compared to White adults (19%). In addition, four in ten Black adults (39%) and a third of Hispanic adults say they know someone who has died from coronavirus, compared with 24% of those who are White.
Black adults who work outside their homes are also disproportionately worried about contracting the virus while at work. Among those who work outside of their home, six in ten Black adults are worried about getting sick from coronavirus while at work (including 34% who are “very worried”), compared with just under half of White adults who are worried (11% “very worried”). Worry rises to seven in ten among Black women who work outside the home (69%) and among working Black adults who live in a household where someone has a serious health condition (71%).
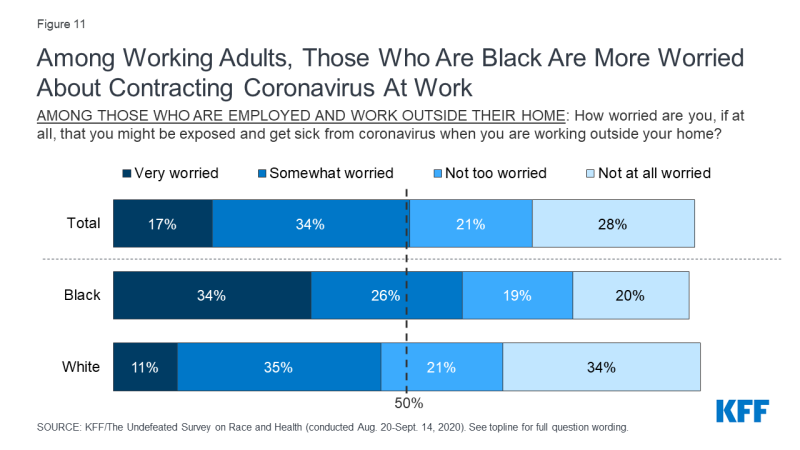
Figure 11: Among Working Adults, Those Who Are Black Are More Worried About Contracting Coronavirus At Work
Two-thirds of Black adults think that the federal government would be taking stronger action to fight the pandemic if White people were getting sick and dying from coronavirus at higher rates than people of color. In contrast, 72% of White people believe the government’s response would not be different. Attitudes among Hispanic adults are more mixed: 42% say the government’s response would be stronger and 47% say it would not be different. These attitudes are also highly partisan, with six in ten Democrats believing the government response would be stronger if more White people were dying and the vast majority (90%) of Republicans saying the response would be no different.

Figure 12: Most Black Adults, Democrats Say Government Pandemic Response Would Be Stronger If More White People Were Affected
Views Of A Potential COVID-19 Vaccine
With planning beginning for an eventual COVID-19 vaccine, one important consideration is making sure that distribution processes and outreach and communication strategies reach people of color. Vaccination among people of color will be particularly important because they are bearing a heavy, disproportionate burden of the disease, and population immunity is not likely to be reached without high vaccination rates across all communities. However, achieving a high vaccination rate will require public health officials and providers to overcome a range of barriers to vaccination among people of color, many of which are rooted in a historic legacy of abuse and mistreatment by the medical system and ongoing racism and discrimination today. The survey findings provide greater insight into these barriers.
The survey finds that Black adults are less likely than other groups to say they would get a coronavirus vaccine if it was free and determined safe by scientists. Half of Black adults say if a coronavirus vaccine was determined to be safe by scientists and available for free to everyone who wanted it, they would “definitely” or “probably” get vaccinated, compared to six in 10 Hispanic adults and 65% of White adults. In fact, just 17% of Black adults say they would “definitely” get the vaccine, 20 percentage points lower than the share of both Hispanic and White adults (37% each).
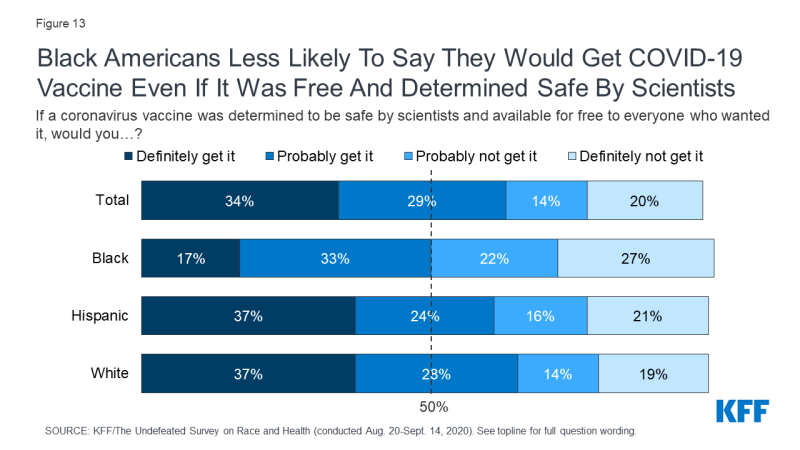
Figure 13: Black Americans Less Likely To Say They Would Get COVID-19 Vaccine Even If It Was Free And Determined Safe By Scientists
The racial differences in willingness to obtain a vaccine widen when partisan differences are taken into account. About three-quarters of Democrats (77%) say they would “definitely” or “probably” get a coronavirus vaccine if it was free and safe, compared to about two-thirds of independents (67%) and just under half of Republicans (47%). Considering both race and partisanship together, the racial divide in vaccine hesitancy among Democrats and independents is stark. Two-thirds (65%) of White Democrats say they would “definitely” get vaccinated, compared with just 23% of Black Democrats. Similarly, among independents, those who are White are more than 3 times as likely to say they would definitely get a vaccine as those who are Black (41% vs. 12%).
| Democrats | Independents | Republicans* | ||||||
| Total | Black | White | Total | Black | White | Total | White | |
| If a coronavirus vaccine was determined to be safe by scientists and available for free to everyone who wanted it, would you…? | ||||||||
| Definitely/Probably get it (NET) | 77% | 55% | 87% | 67% | 48% | 70% | 47% | 50% |
| Definitely get it | 51 | 23 | 65 | 35 | 12 | 41 | 20 | 20 |
| Probably get it | 26 | 33 | 22 | 31 | 36 | 29 | 27 | 30 |
| Definitely/Probably not get it (NET) | 21 | 44 | 10 | 31 | 51 | 29 | 51 | 49 |
| Probably not get it | 12 | 24 | 8 | 12 | 20 | 9 | 20 | 21 |
| Definitely not get it | 9 | 20 | 2 | 20 | 31 | 20 | 31 | 28 |
| * Sample size of Black Republicans insufficient to report separately. | ||||||||
Risk factors appear to play a small role in Black adults’ willingness to obtain the vaccine. Six in ten Black adults ages 65 and over – who are at higher risk for serious illness if they contract coronavirus– say they would probably or definitely get vaccinated if a safe vaccine was available for free, slightly higher than among those under age 65. But, Black adults who live in a household where someone has a serious health condition or works in a health care setting – two other groups at disproportionate risk for serious illness or exposure – are not significantly more likely than their counterparts to say they would be willing to take a vaccine.
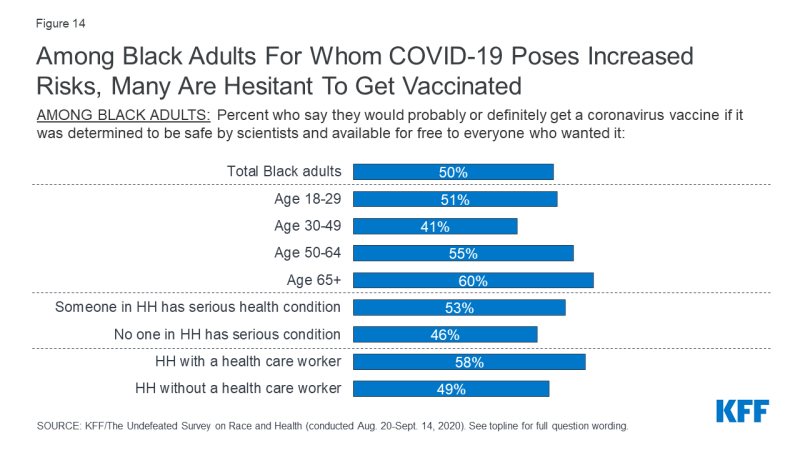
Figure 14: Among Black Adults For Whom COVID-19 Poses Increased Risks, Many Are Hesitant To Get Vaccinated
The racial difference in willingness to take a coronavirus vaccine may at least partially reflect a difference in attitudes towards vaccines in general. Black adults are less likely than their White counterparts to say they usually get a flu vaccine each year (49% vs. 60%). Still, this doesn’t explain the difference entirely, as Black adults who normally get a flu vaccine are 18 percentage points less likely than White adults who normally get a flu vaccine to say they would get a vaccine for coronavirus if it was determined to be safe and freely available (66% vs. 84%).
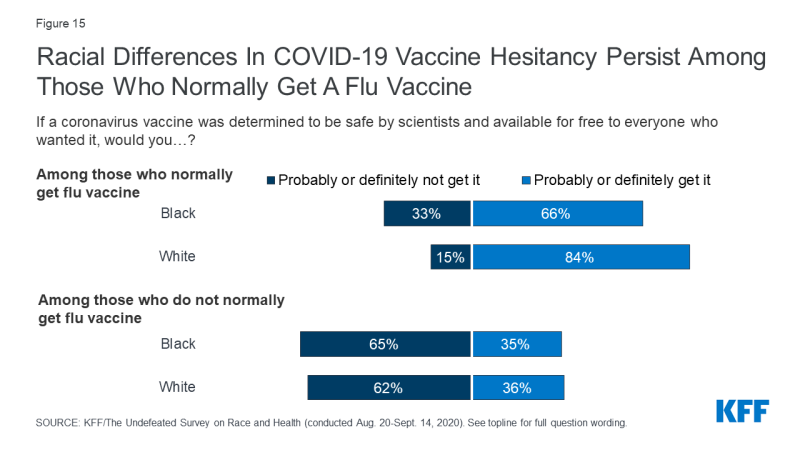
Figure 15: Racial Differences In COVID-19 Vaccine Hesitancy Persist Among Those Who Normally Get A Flu Vaccine
The primary reasons Black adults cite for saying they definitely or probably would not get a coronavirus vaccine are safety concerns and distrust of the health care system. When asked to say in their own words why they would not get a coronavirus vaccine, four in ten Black adults (39%) cite safety concerns, as do three in ten White adults. Thirty-five percent of Black adults who say they won’t get vaccinated cite distrust in either the health care system, the government, or vaccines in general as a reason, higher than the share of White adults who say the same (23%). By contrast, White adults who say they won’t get vaccinated are more likely than Black adults to say they don’t want or need a vaccine or don’t think they’re at risk of getting sick from coronavirus (39% vs. 21%). Six percent of both Black and White adults who say they would not get vaccinated cite concerns about the vaccine development process.
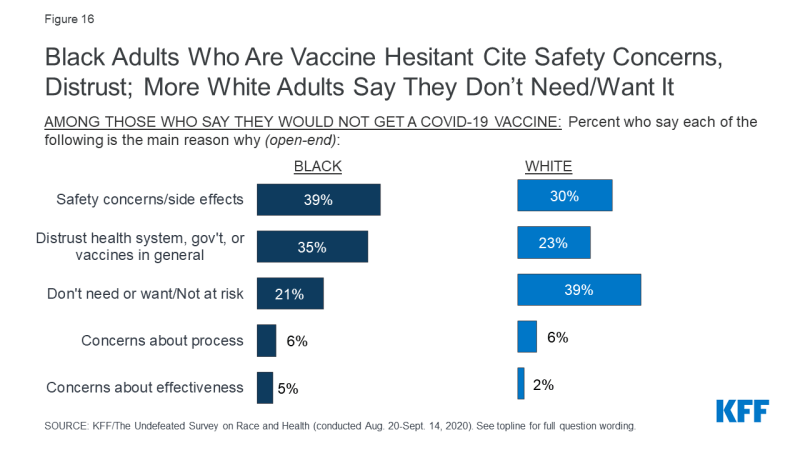
Figure 16: Black Adults Who Are Vaccine Hesitant Cite Safety Concerns, Distrust; More White Adults Say They Don’t Need/Want It
In Their Own Words
Survey respondents’ open-ended answers to the question “What is the main reason why you would not get a vaccine for coronavirus?” reveal the breadth of questions and concerns that people have about a potential vaccine. Some examples are shown below:
Safety concerns/side effects
“Not sure if it would work or could cause some kind of bad reaction or death. I will have to see if it actually works before I take it.” (Black woman, age 65+)
“Because I believe they would be putting the virus in me instead of protecting me from it. …. I would need more proof that it’s safe before I would allow myself or my child to take the vaccine.” (Black woman, age 18-29)
“It’s new. Even if tested, there will be negative impacts.” (White woman, age 30-49)
Distrust of health care system/vaccines/government
“Because I am a Black woman as you know and don’t trust the people who give the vaccine and want [it] to be tested on another race before it’s given to Black people.” (Black woman, age 50-64)
“Do not trust the safety of a vaccine given the current President’s adversarial relationship with the truth and transparency.” (Black man, age 30-49)
“Because it would take a long time for the research to come through, I don’t trust the medical community because of mistakes in the past.” (Black man, age 65+)
Don’t need or want/Not at risk
“I’m healthy. If I get the virus, [I] don’t think there is not much risk to my health.” (Black man, age 30-49)
“I’ve never gotten vaccines and I don’t ever get sick.” (White woman, age 18-29)
“[I] don’t think the coronavirus is as deadly as it is said to be.” (White man, age 50-64)
“I am a Republican, Republicans do not get coronavirus.” (White man, age 65+)
Concerns about development process
“Rush to market. Not taking vaccines through the typical test studies.” (Black woman, age 50-64)
“They’re pushing it too fast because of the president.” (White man, age 65+)
Overall, a majority of Black adults express concerns about whether an eventual vaccine will have been properly tested for safety and effectiveness and whether it will be distributed fairly. Nearly two-thirds (65%) of Black adults are “not at all confident” or “not too confident” that the development of the vaccine is taking the needs of Black people into account. Moreover, six in ten Black adults (61%) say they are “not too confident” or “not at all confident” that an eventual vaccine will have been properly tested for safety and effectiveness, and 66% are not confident that it will be distributed in a way that is fair. By contrast, about half of Hispanic adults and about six in ten White adults say they are at least somewhat confident that a vaccine will be properly tested and that it will be distributed fairly.
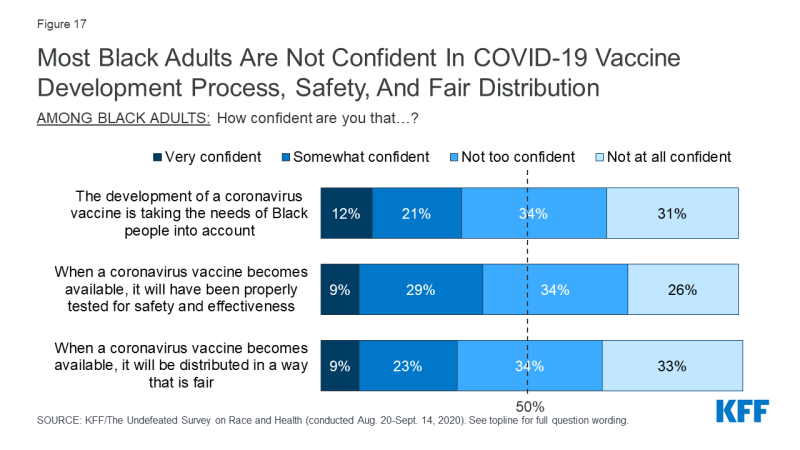
Figure 17: Most Black Adults Are Not Confident In COVID-19 Vaccine Development Process, Safety, And Fair Distribution
Trust And Experiences In The Health Care System
The longstanding and persistent racial disparities in health reflect a variety of factors both within and beyond the health care system, including differences in health insurance coverage, health care access, and social and economic factors that influence health. Moreover, research shows that racial disparities in health persist after controlling for these factors, suggesting that other factors, including historic and ongoing racism and discrimination, play a role in driving these differences. The survey findings provide greater insight into how racism and discrimination shape Black adults’ experiences with the health care system.
Trust of Providers and Hospitals
Reflecting their experiences with discrimination and systemic racism, Black people express lower levels of trust in a variety of organizations and institutions compared to those who are White. The gulf is widest when asked how often they can trust the police to do what is right for them and their community – just 30% of Black adults say they can trust the police “almost all of the time” or “most of the time,” compared with 72% of White adults. A little over half of Hispanic adults (56%) say they can trust the police.
While Black and Hispanic adults are generally more trusting of doctors and hospitals than they are of the police, courts, and schools, there is a racial gap in trust when it comes to health care as well. Compared to White adults, Black adults are 19 percentage points less likely to trust doctors (59% vs. 78%), 14 percentage points less likely to trust local hospitals (56% vs. 70%), and 11 percentage points less likely to trust “the health care system” (44% vs. 55%) to do what is right for them and their communities. On each of these items, the responses for Hispanic adults fall in between those of Black and White adults.
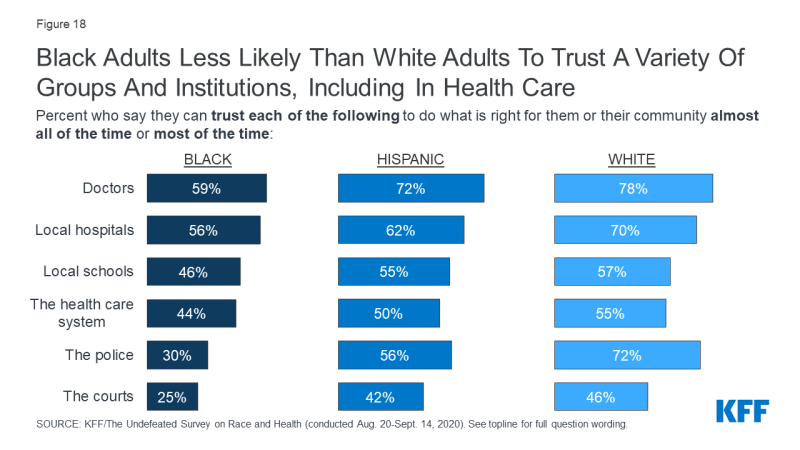
Figure 18: Black Adults Less Likely Than White Adults To Trust A Variety Of Groups And Institutions, Including In Health Care
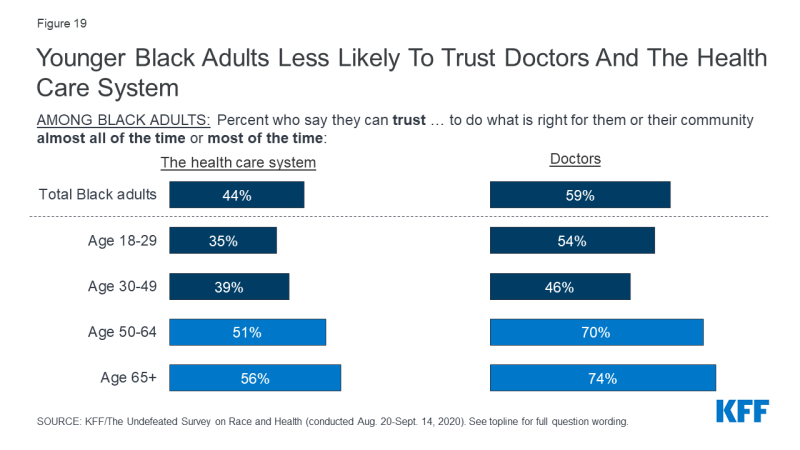
There is an age gap in trust as well, with younger Black adults less likely than their older counterparts to say they trust doctors and the health care system to do what is right for them and their communities. For example, roughly half of Black adults under age 50 say they can trust doctors almost all or most of the time, compared with about 7 in 10 Black adults ages 50 and over.
Perceptions of Unfair Treatment in Health Care
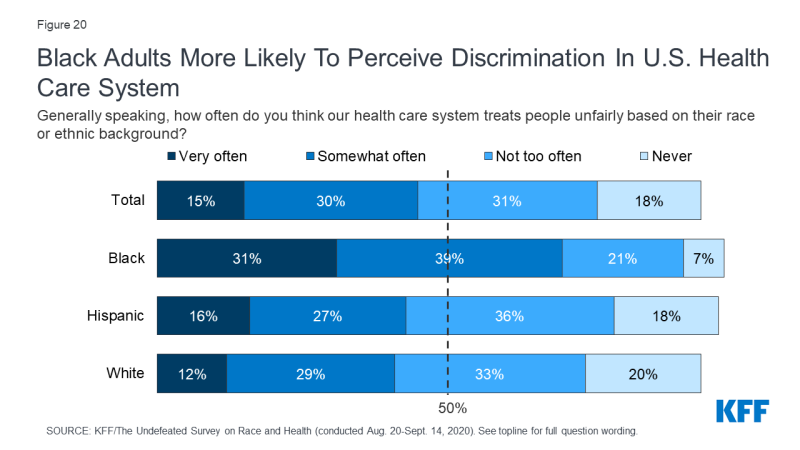
Most Black adults feel the health care system treats people unfairly based on their race or ethnic background, and this share has increased over time. Fully seven in ten Black adults say that “our health care system treats people unfairly based on their race or ethnic background” very often or somewhat often, compared to 41% of White adults and 43% of Hispanic adults.
The share of Black adults who believe race-based discrimination in health care happens very or somewhat often has increased over the past 20 years (from 56% in 1999 to 70% now), while the shares among Hispanic and White adults have remained statistically similar to what they were in 1999.
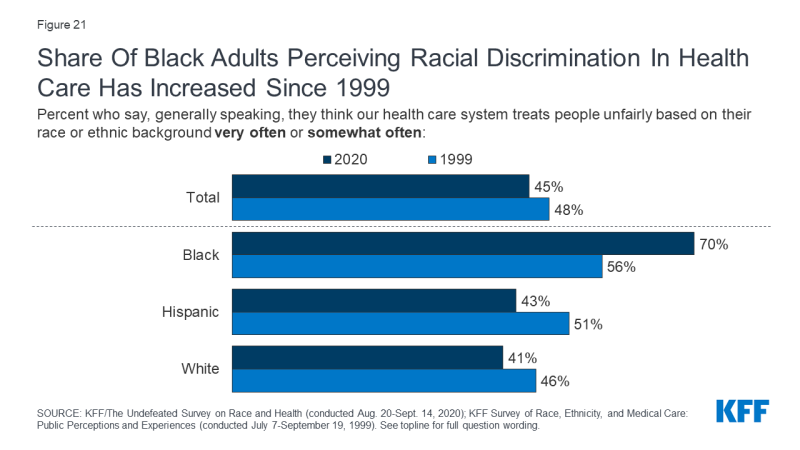
Figure 21: Share Of Black Adults Perceiving Racial Discrimination In Health Care Has Increased Since 1999
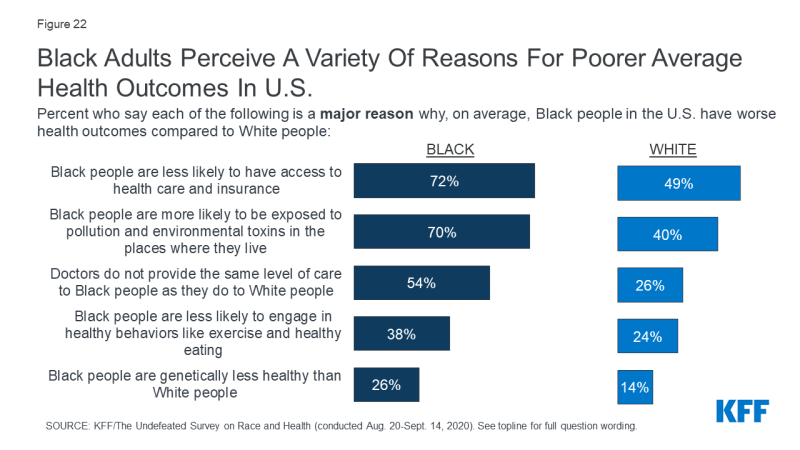
Black adults identify a range of reasons why Black people have worse average health outcomes compared to White people. When asked about potential reasons why Black people in the U.S. have worse outcomes on average compared to White people, Black adults are much more likely than White adults to view various factors as major reasons, including disparities in access to health care and insurance (72% vs. 49%), environmental exposures (70% vs. 40%), and disparities in the level of care provided to Black vs. white patients (54% vs. 26%). Black adults are also somewhat more likely than their White counterparts to blame lack of healthy behaviors (38% vs. 24%) and genetic differences (26% vs. 14%) for racial disparities in health outcomes. The perception of the role of genetic differences stands in contrast to research disproving biologic differences as a driver of racial disparities in health; moreover, there is growing recognition that individual health behaviors are influenced by policies, systems, and environments.
Experiences With and Access to Health Care Providers
A significant and longstanding body of research suggests that provider and institutional bias and discrimination are drivers of racial disparities in health, contributing to racial differences in diagnosis, prognosis, and treatment decisions. Research further points to the role of communication and interactions between providers and patients and suggests that enhancing providers’ ability to provide culturally and linguistically appropriate care as well as increasing diversity of the health care workforce may help address disparities in health. Reflecting these factors, studies show, for example, that people of color receive lower quality of care, receive less adequate treatment for acute and chronic pain, and report higher rates of mistreatment during the course of their pregnancy. Pointing to the importance of culturally competent care, one recent study found that there were significant improvements in mortality for Black newborns who were cared for by Black physicians. Beyond these factors, people of color may face increased difficulty accessing care due to cost or lack of easily accessible providers, among other factors. The survey findings provide greater insight into individuals experiences with health care providers and their ability to access providers, including those with a shared background and experience.
One in five Black and Hispanic adults report they were personally treated unfairly because of their race and ethnicity while getting health care in the past year, with higher shares among younger Black adults and women, particularly mothers. Twenty percent of Black adults and 19% of Hispanic adults say they were personally treated unfairly because of their race or ethnicity when getting health care for themselves or a family member in the past 12 months, while just 5% of White adults say this has happened to them. Younger Black adults (23% of those ages 18-29 and 28% of those ages 30-49) and Black women (25%) are more likely than older Black adults to report being treated unfairly when receiving care. Among Black mothers of children under age 18, nearly four in ten (37%) say they have been treated unfairly in the past 12 months while getting health care for themselves or a family member. Familiarity with the medical community also does not appear to shield Black adults from discrimination in health care settings; 34% of those who work in a health care delivery setting or live with someone who does say they’ve experienced race-based discrimination while getting health care in the past year.
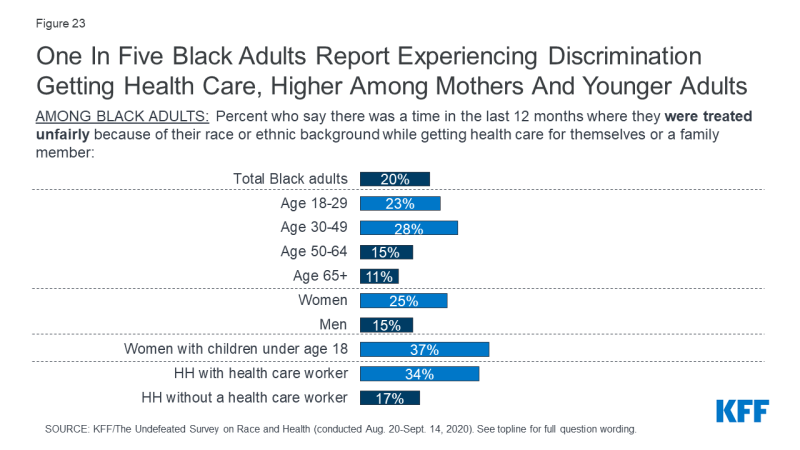
Figure 23: One In Five Black Adults Report Experiencing Discrimination Getting Health Care, Higher Among Mothers And Younger Adults
In addition to reporting being treated unfairly, an even larger share of Black adults – 36% – say there was a time in the past few years when they think they would have gotten better medical care if they belonged to a different race or ethnic group. Mirroring age patterns of reported discrimination, Black adults under age 50 are more likely than those ages 50 and over to feel they would have gotten better care if they were a different race.
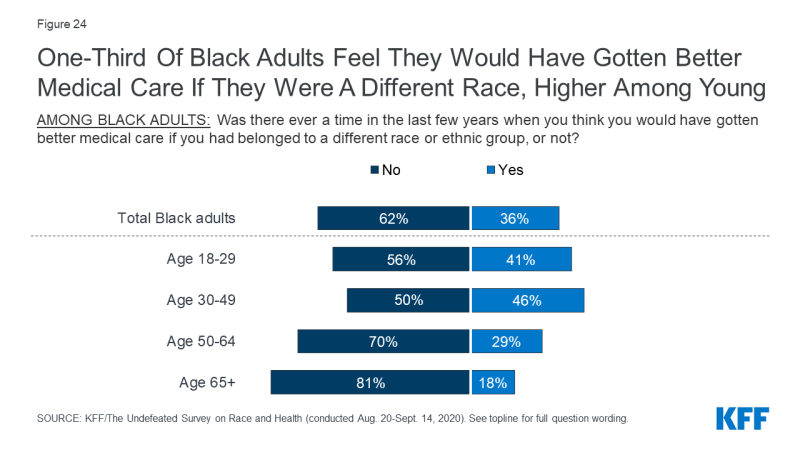
Figure 24: One-Third Of Black Adults Feel They Would Have Gotten Better Medical Care If They Were A Different Race, Higher Among Young
Across racial and ethnic groups, many adults report having some specific negative experiences with health care providers. Overall, about a quarter of adults say that in the past 3 years, a doctor or other health care provider has assumed something about them without asking (24%) or talked down to them or treated them without respect (23%). Just under one in five say there was a time in the past 3 years when a provider didn’t believe they were telling the truth (19%) or suggested they were personally to blame for a health problem (17%). About one in seven say a doctor refused to order a test or treatment (14%) or pain medication (13%) they thought they needed.

Figure 25: Nearly Half Of Adults Overall Report One Of Six Negative Experiences With Health Care Providers In Last 3 Years
Black adults are more likely than White adults to report some negative experiences with health care providers. These differences include feeling that a provider didn’t believe they were telling the truth (22% of Black adults vs. 17% of White adults say this happened to them in the past 3 years), being refused a test or treatment they thought they needed (19% vs. 12%), and being refused pain medication (18% vs. 13%). Other negative experiences were reported at similar rates among Black and White adults, including health care providers suggesting they were personally to blame for a health problem, assuming things without asking, and treating them with a lack of respect. About half of Black adults (49%), a similar share of White adults (45%), and four in ten Hispanic adults (39%) report experiencing at least one of these things in the past 3 years. Together, these findings suggest that across groups, patients encounter negative experiences obtaining care, but Black people are more likely to report negative experiences in some specific instances.
Interestingly, most Black adults who experienced at least one form of mistreatment do not believe their race was a factor. About four in ten (38%) of those who had at least one negative experience (19% of all Black adults) think it happened specifically because of their race, while the majority (27% of all Black adults) say it was for some other reason.
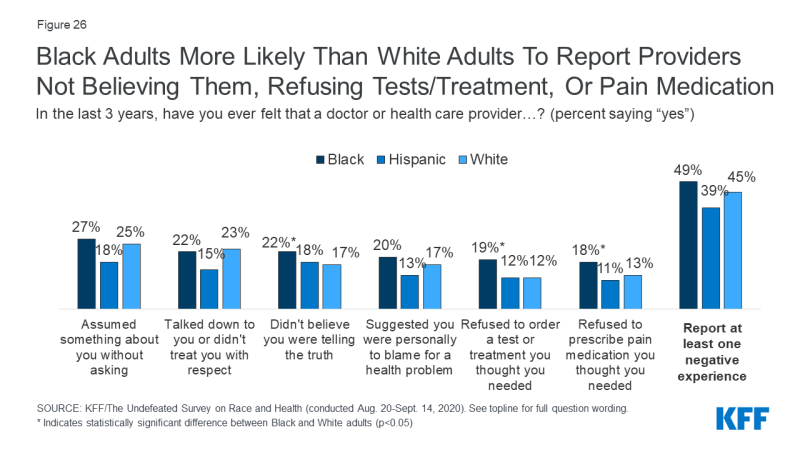
Figure 26: Black Adults More Likely Than White Adults To Report Providers Not Believing Them, Refusing Tests/Treatment, Or Pain Medication
In addition to differences by race, there are also gender differences in the treatment people report receiving from health care providers. Black women are more likely than Black men to report feeling that a health care provider didn’t believe they were telling the truth (27% vs. 16%), assumed something without asking (32% vs. 22%), talked down or treated them without respect (27% vs. 17%), or suggested they were personally to blame for their health problems (24% vs. 15%). Among Black women with children, the share who say a health care provider talked down to them or treated them with disrespect rises to 41%.
In most cases, there are similar gender gaps between the experiences of White women and men as well, though when it comes to being personally blamed for their health problems, the opposite pattern is true, with White men more likely than White women to report this experience.
| In the last 3 years, have you ever felt that a doctor or health care provider…? (percent saying “yes”) | Total | Black | White | |||
| Women | Men | Women | Men | Women | Men | |
| Assumed something about you without asking | 29%* | 20% | 32%* | 22% | 29%* | 21% |
| Talked down to you or didn’t treat you with respect | 27* | 19 | 27* | 17 | 27* | 19 |
| Didn’t believe you were telling the truth | 23* | 15 | 27* | 16 | 20* | 13 |
| Suggested you were personally to blame for a health problem you were experiencing | 16 | 19 | 24* | 15 | 13 | 20* |
| Refused to order a test or treatment you thought you needed | 17* | 11 | 20 | 17 | 14 | 10 |
| Refused to prescribe pain medication you thought you needed | 14 | 13 | 20 | 16 | 12 | 13 |
| Experienced at least one of the above | 49* | 42 | 52 | 45 | 47 | 43 |
| * indicates statistically significant difference between men and women within group. | ||||||
Black and Hispanic adults are more likely than their White counterparts to say it’s difficult to find a doctor who shares their background and experiences and one who treats them with dignity and respect. About two-thirds (65%) of Black adults and over half (54%) of Hispanic adults say it is very or somewhat difficult for them to find a doctor who shares their background and experiences, while most White adults (53%) say this is easy. Similarly, about one in five adults who are Black (21%) or Hispanic (22%) say it is difficult to find a doctor who treats them with dignity and respect, compared to a smaller share of those who are White (14%).
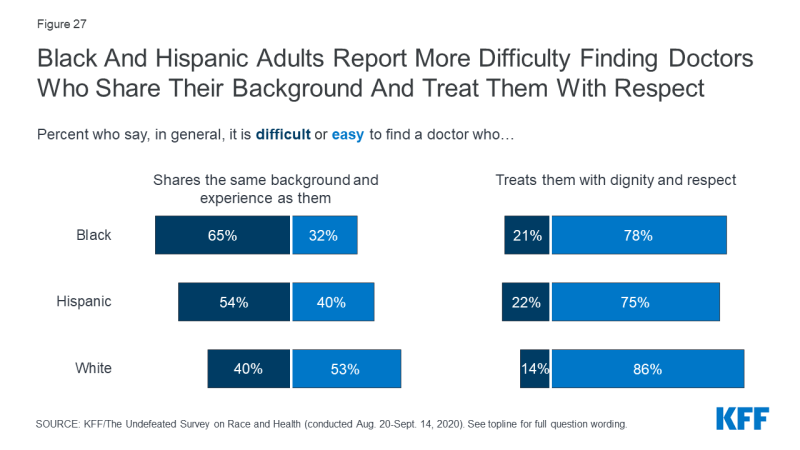
Figure 27: Black And Hispanic Adults Report More Difficulty Finding Doctors Who Share Their Background And Treat Them With Respect
Among White adults, those with college degrees are much more likely than those without a degree to say it’s easy to find a doctor who shares their background and experience. However, this education advantage does not exist among Black adults. Nearly two-thirds (64%) of Black adults with a college degree say it’s difficult to find a doctor who shares their background and experience, about two and a half times the rate among college-educated White adults (27%). The pattern is similar across income groups – higher-income White adults are more likely than those with lower incomes to say it is easy to find a provider who shares their background and experiences, while about two-thirds of Black adults across income groups say it is difficult.
| How easy or difficult is it to find a doctor who shares the same background and experience as you? | Black | White | ||
| No 4-year degree | College graduate | No 4-year degree | College graduate | |
| Very/somewhat easy | 31% | 35% | 47% | 64% |
| Very/somewhat difficult | 66 | 64 | 48 | 27 |
| Don’t know/Refused | 3 | 1 | 5 | 10 |
| How easy or difficult is it to find a doctor who shares the same background and experience as you? | Black | White | ||||
| <$40K | $40-$89.9K | $90K+ | <$40K | $40-$89.9K | $90K+ | |
| Very/somewhat easy | 33% | 31% | 33% | 44% | 53% | 65% |
| Very/somewhat difficult | 65 | 67 | 67 | 52 | 39 | 32 |
| Don’t know/Refused | 2 | 2 | 1 | 4 | 8 | 3 |
For Black and Hispanic Americans, finding a doctor who shares their background and experience may or may not mean seeing a doctor of the same race or ethnicity. In fact, about one quarter (24%) of Black adults say they would prefer to see a Black doctor, while most say it doesn’t make much difference. Still, 24% of Black adults say they’ve never received care from a Black doctor, including 35% of those ages 18-29 and 28% of those who say they would prefer to see a doctor who is Black. A similar 28% of Hispanic adults say they’ve never received care from a doctor who is Hispanic or Latino.
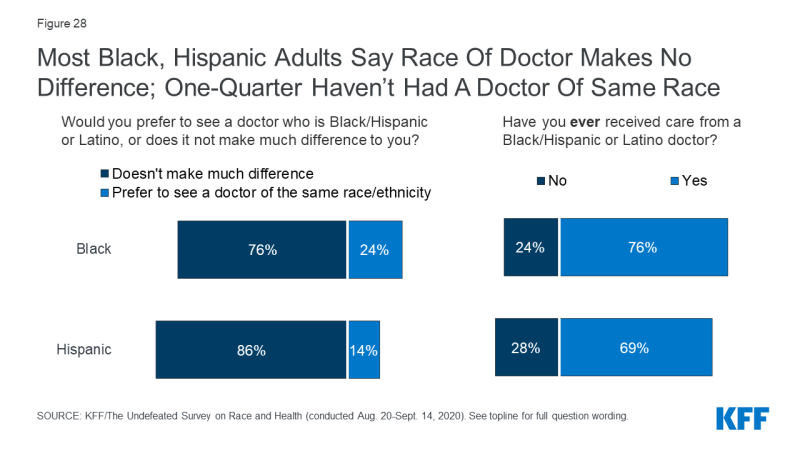
Figure 28: Most Black, Hispanic Adults Say Race Of Doctor Makes No Difference; One-Quarter Haven’t Had A Doctor Of Same Race
Black and Hispanic adults are more likely than White adults to report financial and accessibility barriers to obtaining health care. About half of Black (48%) and Hispanic (49%) adults say it is very or somewhat difficult to find health care they can afford, compared to a somewhat smaller share of White adults (39%). Similarly, about a quarter (24%) of Black adults and three in ten Hispanic adults say it is difficult to find health care at a location that is easy for them to get to, compared to 18% of White adults.
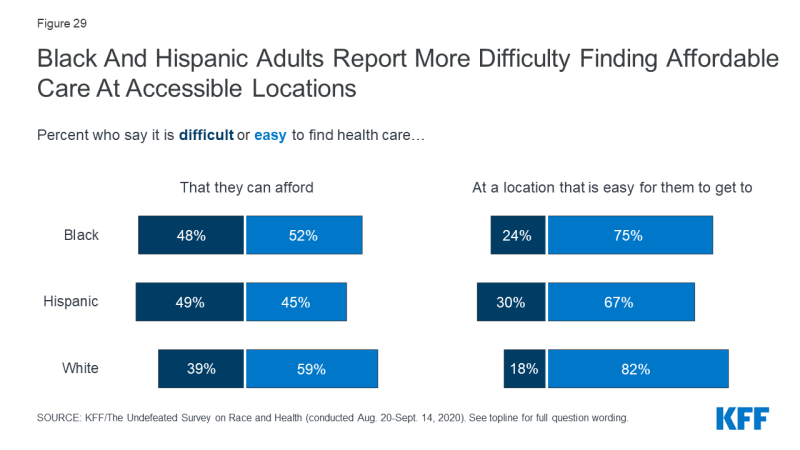
Figure 29: Black And Hispanic Adults Report More Difficulty Finding Affordable Care At Accessible Locations
The differences between Black and White adults on these questions are largely driven by income differences. That is, those with lower incomes generally report more difficulty finding accessible and affordable care than those with higher incomes, and Black and White adults at similar income levels report similar levels of difficulty on both these measures.
| How easy or difficult is it to find health care you can afford? | Black | White | ||||
| <$40K | $40-$89.9K | $90K+ | <$40K | $40-$89.9K | $90K+ | |
| Very/somewhat easy | 46% | 57% | 64% | 49% | 60% | 70% |
| Very/somewhat difficult | 54 | 43 | 34 | 48 | 38 | 28 |
| How easy or difficult is it to find health care at a location that is easy for you to get to? | ||||||
| Very/somewhat easy | 73 | 77 | 86 | 73 | 87 | 87 |
| Very/somewhat difficult | 27 | 22 | 13 | 26 | 13 | 13 |
| Note: There were not enough Hispanic respondents in the survey to provide similar income breaks. | ||||||
Conclusion
These survey findings highlight some of the many challenges facing Black individuals and families in 2020. Black people in the U.S. are bearing a heavy burden of the health and economic consequences of the COVID-19 pandemic, and the survey shows the pandemic is taking an unequal toll on their financial stability, their ability to care for their children, and their emotional well-being. The findings further illustrate that, once a COVID-19 vaccine becomes available, accomplishing a high vaccination rate will require addressing multiple barriers to vaccination among the Black community, including building public trust and willingness to obtain the vaccine by addressing distrust and safety concerns.
In addition, despite longstanding research documenting racial health disparities, the survey shows that racism and discrimination still play a major role in shaping people’s perceptions and experiences with obtaining health care. Most Black adults believe that race-based discrimination in health care happens at least somewhat often, and they are more likely compared to White adults to report experiencing specific negative experiences with health care providers. Many of these experiences are even more common among Black women, particularly those with children. Black adults also face difficulties finding providers who share their background and experiences and treat them with dignity and respect, as well as challenges finding health care they can afford and easily access – challenges shared by Hispanic adults. These findings point to the importance of continuing to prioritize equity in health care, and, in particular, efforts to address individual and institutional bias and discrimination and social and economic inequities that increase barriers to health.
[ad_2]
Source link