Army builds tool to save lives at high altitude | Article

[ad_1]

Volunteers from the 3rd Armored Brigade Combat Team, 1st Division, in Fort Bliss, Texas, donned four real-time physiologic monitors for 68 hours, to measure peripheral oxygen saturation, heart rate, energy expenditure and sleep quality at the Taos Ski Valley, New Mexico, in August, as part of the U.S. Army Research Institute of Environmental Medicine’s research study to validate the AMS_alert algorithm, a tool that will predict Acute Mountain Sickness in real time in individuals prior to occurrence in order to give an alert or warning such that treatment, evacuations, and mission planning can occur in a safe manner.
VIEW ORIGINAL
NATICK, Mass. — Mountain climbing is risky business. When unacclimatized individuals rapidly ascend to altitudes greater than 8,000 feet, they put themselves at risk for suffering from high-altitude illnesses. The addition of hard physical exercise, typical of a military mission, increases this level of risk. Detecting these illnesses prior to occurrence has the potential to save lives.
The U.S. Army Research Institute of Environmental Medicine, or USARIEM, researchers recently returned from Taos Ski Valley, New Mexico, where they completed their data collection for the AMS_alert algorithm, a tool that will predict acute mountain sickness in individuals prior to occurrence.
Thirty-eight Warfighters from the 3rd Armored Brigade Combat Team, 1st Division, at Fort Bliss, Texas, volunteered their time in August to participate in this research this past summer. The data collected from this study is a continuation of the Taos Ski Valley study completed in the summer of 2021 with 41 Warfighters from the 5th Engineer Battalion at Fort Leonard Wood, Missouri.

Volunteers from the 3rd Armored Brigade Combat Team, 1st Division, in Fort Bliss, Texas, took part in daily hikes to 12,400 feet at the Taos Ski Valley, New Mexico, in August, as part of the U.S. Army Research Institute of Environmental Medicine’s research study to validate the AMS_alert algorithm, a tool that will predict Acute Mountain Sickness in real time in individuals prior to occurrence in order to give an alert or warning such that treatment, evacuations, and mission planning can occur safely.
VIEW ORIGINAL
“This tool has the potential to save lives at high altitude and identify high-risk individuals before a casualty occurs,” said Dr. Beth Beidleman, research physiologist with USARIEM’s Military Performance Division. “AMS can progress into life-threatening high-altitude pulmonary edema [HAPE] or high-altitude cerebral edema [HACE] which both require evacuation. Both of these illnesses involve fluid either in the lungs or brain and can result in death within 24 hours.”
One Soldier in last summer’s study experienced all three high-altitude illnesses – AMS, HAPE and HACE.
“Fortunately, we were able to evacuate this volunteer to the nearest emergency room and there were no untoward or lasting effects, but this option is not always available when Warfighters are on a mission in remote mountainous regions,” said Beidleman. “Having a hypoxia monitoring system on board can be the difference between life and death.”
Roughly 50 to 90 percent of unacclimatized Warfighters will experience AMS symptoms when rapidly ascending to high altitudes greater than 8,000 feet, depending on the altitude. AMS can impact every aspect of a Warfighter’s physical and mental performance.

Volunteers from the 3rd Armored Brigade Combat Team, 1st Division, in Fort Bliss, Texas, hiked 3.1 miles up a 15.5 percent mean grade gravel road with a weighted backpack, ascending from 9,000 feet to 11,800 feet, in Taos Ski Valley, New Mexico, in August, as part of the U.S. Army Research Institute of Environmental Medicine’s research study to validate the AMS_alert algorithm, a tool that will predict Acute Mountain Sickness in individuals prior to occurrence.
VIEW ORIGINAL
“If we can alert commanders and non-commissioned officers on the field in real-time that someone is in trouble prior to occurrence of AMS, HAPE or HACE, they can begin treatment early, adjust the mission, and plan evacuations safely.”
Warfighters arrived at the Taos Ski Valley, 9,000 feet above sea level, at the end of July to participate in the 4-day study. From there, they either hiked with a weighted backpack or were driven to 11,800 feet. Unlike other environments, the dismounted Warfighter is the primary weapon platform at altitude, and the impact of hard physical exercise during ascent is understudied. One aim of this research study was to answer whether hard exercise during altitude ascent impacts the timing and severity of high-altitude illnesses.
“The preliminary results suggest that active ascent induces sickness earlier in the exposure and more extreme forms of altitude illness are observed,” said Beidleman.
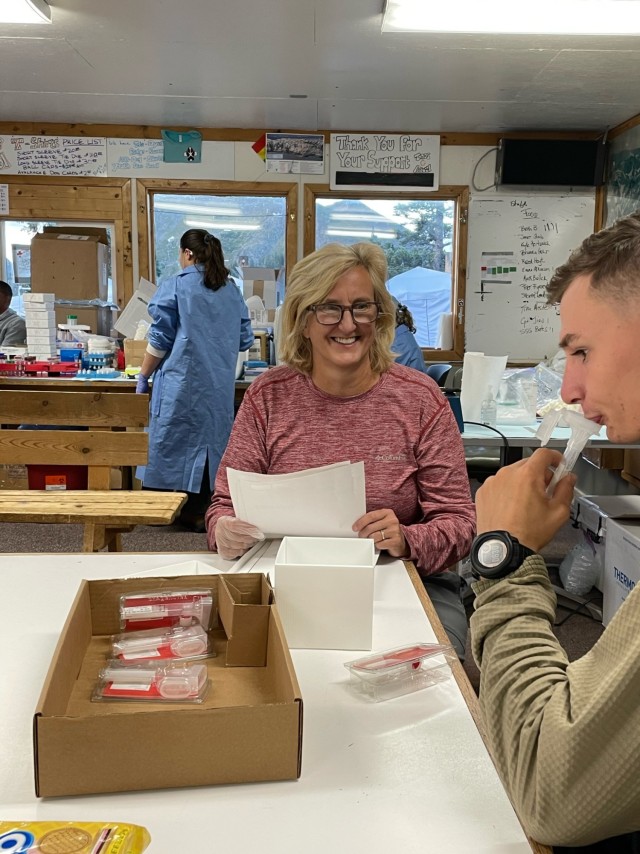
Dr. Beth Beidleman, principal investigator with the U.S. Army Research Institute of Environmental Medicine’s Military Performance Division, takes saliva samples of a volunteer from the 3rd Armored Brigade Combat Team, 1st Division, in Fort Bliss, Texas, in order to identify potential genomic markers of Acute Mountain Sickness. Volunteers completed data collection in August at the Taos Ski Valley, New Mexico, at 11,800 feet, a strategically important altitude that has a high likelihood of military deployment.
VIEW ORIGINAL
In addition, most Warfighters live below 12,000 feet when deployed to altitude, and the majority of altitude research occurs at altitudes above 14,000 feet. The results, therefore, have strategic military relevance. This is the largest altitude study, with 79 participants, conducted by USARIEM in the 60-year history of the institute. This study is historically significant due to the simulation of a military mission at altitude with hard exercise during ascent, and the number of diverse Warfighters studied.
During the study, participants wore four monitors. The first monitor, a chest strap developed at USARIEM, was worn to measure heart rate and skin temperature. Second was a pulse oximeter attached to the wrist with a sensor on the finger for peripheral oxygen saturation. Third, a sleep watch was used to measure sleep quality and quantity. The fourth monitor was an ankle accelerometer to measure energy expenditure over the 68 hours of the study.
The participants wore all sensors for 68 hours — the total time of the study — to capture their response to the altitude ascent.
“There is a huge interindividual variability in response to altitude ascent,” explains Beidleman. “Some individuals get sick and others do not. Physiologic markers of acclimatization, such as heart rate, peripheral oxygen saturation and hemoglobin concentration, may account for these differences. Some individuals produce proteins that improve adaptive responses to altitude while others do not based on their genomic profile, which may explain why different people respond differently.”

Emma Atkinson, biomedical engineer with the U.S. Army Research Institute of Environmental Medicine’s Military Performance Division, takes the temperature of a volunteer from the 3rd Armored Brigade Combat Team, 1st Division, in Fort Bliss, Texas, to screen for potential symptoms of COVID-19, during USARIEM’s research study to validate the AMS_alert algorithm, a tool that will predict Acute Mountain Sickness in individuals prior to occurrence in August. Upper respiratory infections may increase the severity of high-altitude illnesses due to compromised oxygen transport in a limited oxygen environment.
VIEW ORIGINAL
The participants were a diverse group, comprising 40 percent Caucasian, 30 percent African American and 30 percent Hispanic American or mixed heritage. Ten percent of the volunteers were women. In previous years, it was typically 90 percent Caucasian.
Preliminary findings from the first year suggest Hispanic Americans are most protected against AMS, African Americans are the least protected against AMS, and Caucasians fall in between these two groups.
“The prediction algorithm should be robust for everyone, which is the reason for the big sample size and data collection efforts over a two-year period.” said Beidleman.
Beidleman continued explaining that currently, the accuracy of the algorithm is 85 percent, with physiologic monitoring alone. With the addition of genomic markers, we hope to increase the accuracy to close to 95 percent.
Preliminary work with Dr. Rasha Hammamieh and her team at the Walter Reed Army Institute of Research suggests that genomic markers can predict who is more susceptible to AMS from blood samples collected at sea level with 100 percent accuracy. One of this study’s aims is to confirm these genomic results.
Data collection is complete, and the results are being analyzed to verify the accuracy of the original AMS_alert algorithm. Plans for including a risk factor score based on protein markers and developing a peripheral oxygen sensor that does not sit on the finger and is more acceptable to the Warfighter are currently underway.

The U.S. Army Research Institute of Environmental Medicine researchers were joined on a daily hike by Warfighters volunteering from the 3rd Armored Brigade Combat Team, 1st Division, in Fort Bliss, Texas, at the Taos Ski Valley, New Mexico as part of the research study to examine the impact of exercise on the incidence and severity of Acute Mountain Sickness.
VIEW ORIGINAL
“When we deploy the algorithm in FY24 through a transition agreement with the U.S. Army Medical Materiel Development Activity, it has the potential to save lives but work still needs to be done on developing a user-acceptable oxygen sensor,” said Beidleman. “The entire hypoxia monitoring system to include an oxygen sensor, validated algorithm and smart phone application will not be delivered until FY26, if critical funding is provided.”
Over the next few years, USARIEM plans to test oxygen sensors to find the best one. Then the validated algorithm will be embedded into a smartphone that will provide an alert on the likelihood of a Soldier experiencing AMS in the next four to eight hours. The final product will then be field tested by the U.S. Army Forces Command and the U.S. Special Operations Command during high-altitude deployments.
Warfighters operate in every terrain, elevation, climate and in any-and-all conditions. The AMS_alert algorithm provides a technological breakthrough in physiologic and genomic monitoring not only for the U.S. Army but also for civilian health-care providers, mountaineers, recreational athletes, and search and rescue teams. This tool is just one of many in the Army modernization effort to optimize the health and performance of our U.S. Military.
━━━━━━━━━━━━━━━
USARIEM is a subordinate command of the U.S. Army Medical Research and Development Command under the Army Futures Command. USARIEM is internationally recognized as the DOD’s premier laboratory for Warfighter health and performance research and focuses on environmental medicine, physiology, physical and cognitive performance, and nutrition research. Located at the Natick Soldier Systems Center in Natick, Massachusetts, USARIEM’s mission is to optimize Warfighter health and performance through medical research.
[ad_2]
Source link
