Denosumab Superior to Alendronate for Reduction of Postmenopausal Fracture Risk in Real-world Study

[ad_1]
In postmenopausal women, treatment with denosumab injection was associated with greater reductions in fracture risk compared with oral alendronate, according to new data from a real-world study presented at the 2023 World Congress on Osteoporosis, Osteoarthritis and Musculoskeletal Diseases, May 4-7, 2023.
In the study of nearly 500 000 women, denosumab, a RANK Ligand inhibitor, was also associated with greater reductions in fracture risk over time than the oral bisphosphonate. Further, longer duration of denosumab treatment yielded greater improvements in fracture risk reduction, according to an Amgen news release.
The retrospective, observational study evaluated data from US Medicare beneficiaries from January 1, 2012, to December 31, 2018. The study cohort comprised 478 651 postmenopausal women aged ≥66 years with no history of prior osteoporosis treatment who received either denosumab (n=89 115) or oral alendronate (n=389 536). Participants were evaluated from treatment initiation to first occurrence of a fracture outcome, medication switch or discontinuation, disenrollment from Medicare, or death.
Investigators reported that denosumab reduced the relative risk (RR) of fracture vs oral alendronate across fracture types, with:
- 36% reduced risk of hip fractures (RR, 0.64; 95% CI, 0.39-0.90)
- 43% reduced risk of nonvertebral fractures, including fractures to the hip, humerus, pelvis, radius/ulna and other femur (RR, 0.57; 95% CI, 0.42-0.71)
- 30% reduced risk of hospitalized vertebral fractures, (RR, 0.70; 95% CI, 0.40-1.01; not statistically significant)
- 39% reduced risk of major osteoporotic nonvertebral and hospitalized vertebral fractures (RR, 0.61; 95% CI, 0.48-0.74)
- 50% reduced risk of non-hip, nonvertebral fractures (RR, 0.50; 95% CI, 0.35-0.64)
The study findings also demonstrated that longer duration of treatment with denosumab led to a greater reduction in risk of major osteoporotic (MOP) fracture: 9% at 1 year (RR, 0.91; 95% CI, 0.85-0.97), 12% at 2 years (RR, 0.88; 95% CI, 0.83-0.93), 18% at 3 years (RR, 0.82; 95% CI, 0.77-0.87), 31% at 5 years (RR, 0.69; 95% CI, 0.62-0.76), and 39% overall (RR, 0.61; 95% CI, 0.48-0.74).
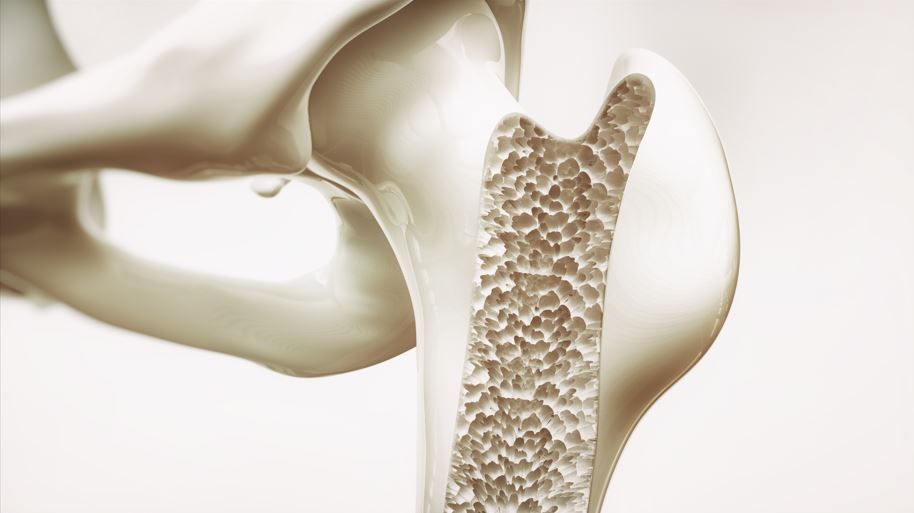
Globally, 1 in 3 women aged >50 years will sustain an osteoporosis-related fragility fracture, with number expected to climb as the population ages. Research shows, however, that there is a large gap in osteoporosis management and treatment, particularly in the post-fracture setting where 4 out of 5 women remain undiagnosed and untreated.
Research shows that there is a large gap in osteoporosis management and treatment, particularly in the post-fracture setting where 4 out of 5 women remain undiagnosed and untreated.
Our study findings “from nearly half a million patients provide evidence that Prolia is associated with greater fracture risk reduction than with alendronate,” said lead study investigator Jeff Curtis, MD, MS, MPH, professor of medicine in the Division of Clinical Immunology and Rheumatology at the University of Alabama at Birmingham. “This comparative effectiveness research employs rigorous methodology that provides important insights that are relevant to the care of women living with osteoporosis.”
[ad_2]
Source link
