Endometriosis symptoms and their impacts

[ad_1]
Plain Language Summary
In this study, 40 US women with endometriosis-associated pain were interviewed about their personal experiences with endometriosis and how it impacts their daily lives. Women were asked open-ended questions (eg, “How did endometriosis affect your life?”) so that they could describe their experiences in their own words. Transcripts of the interviews were assessed to identify the main symptoms of endometriosis described, as well as their impact on daily life.
In total, 18 different symptoms of endometriosis were mentioned across the interviews. Of these, pelvic pain, pain during intercourse (dyspareunia), and heavy menstrual bleeding were the most commonly reported ones; these were described by more than 75% of women interviewed. Women reported that endometriosis symptoms impacted multiple aspects of life: physical (eg, needing to lie down), activities of daily living (eg, unable to do jobs around the house), social (eg, unable to attend social events), sleep (eg, difficulties with sleeping due to endometriosis symptoms), emotional (eg, unable to cope), appearance (eg, being/feeling bloated), financial (eg, cost of surgery), sex-related (eg, negative impact on romantic relationships), work/school-related (eg, missing work/school), fertility-related (eg, difficulty conceiving), and cognitive function (eg, difficulty concentrating or remembering).
This interview study of US women with endometriosis-associated pain adds to the evidence of the burden of endometriosis, from the perspective of affected women, and demonstrates the adverse and debilitating impacts of endometriosis symptoms on daily life.
Introduction
Endometriosis is a chronic, painful, estrogen-driven condition in women, characterized by the growth of endometrial tissue outside the uterus, resulting in an inflammatory response leading to the accumulation of scar tissue.1,2 Endometriosis affects as many as 1 in 10 women during reproductive years;2,3 the exact prevalence is difficult to determine due to underdiagnosis, misdiagnosis, and diagnostic delays.4,5 An endometriosis prevalence of approximately 30% was reported in women of childbearing age with infertility.6 The incidence of endometriosis in the US is highest in women aged 36–45 years, with no differences by race and ethnicity.7
Frequently reported endometriosis symptoms include dysmenorrhea (painful periods), non-menstrual pelvic pain (NMPP), and dyspareunia (pain during intercourse).1,4 Evidence suggests that endometriosis symptoms may have a profound impact on the lives of those affected, including a reduction in quality of life, physical activity and work productivity.8–10 Considering interindividual variability in the clinical presentation of endometriosis,11 this interview study evaluated personal experiences and perceptions of endometriosis symptoms and their impacts on daily life in women in the US. The study aimed to assess the broad range of endometriosis symptoms and impacts as described by women in their own words and to identify aspects of the disease that care providers may not readily discuss with patients. The relationship between endometriosis-associated pain and menstruation was also investigated.
Materials and Methods
Study Design and Eligibility Criteria
This interview-based study was conducted in a sample of US women enrolled in the SPIRIT 1 (ClinicalTrials.gov identifier: NCT03204318) and SPIRIT 2 (NCT03204331) trials. SPIRIT 1 and SPIRIT 2 were Phase 3, randomized, double-blind, placebo-controlled, multinational studies evaluating once-daily relugolix combination therapy (relugolix 40 mg, estradiol 1 mg, and norethindrone acetate 0.5 mg), versus placebo, in women with endometriosis-associated pain through 24 weeks.12 The studies enrolled premenopausal women (aged 18–50 years) with surgically diagnosed endometriosis (with direct visualization and/or histopathologic confirmation of endometriosis), and with moderate-to-severe NMPP and dysmenorrhea.
Target enrollment was 40 US women who had completed Week 24 of SPIRIT 1 or 2, had consented to participate in the interviews, were able to speak, read, write, and understand English, and had completed patient-reported outcome measures assessing endometriosis symptoms (including the Patient Global Assessments for NMPP, dysmenorrhea, and function at baseline). Women were eligible to participate irrespective of treatment assignment and treatment response in the SPIRIT trials.
The interview study was submitted to the Advarra Institutional Review Board for ethics review and approval prior to contact with participants. Participant informed consent included publication of anonymized responses. SPIRIT 1 and SPIRIT 2, from which women were enrolled, were Institutional Review Board-approved studies conducted in accordance with International Conference on Harmonisation guidelines and ethical principles of the Declaration of Helsinki.12
Interviews
Interviews were scheduled to occur within 3–14 days after the Week 24 study visit and were performed prior to unblinding of the SPIRIT trials. Trained interviewers conducted the interviews via web/Internet-based video platform or telephone and audio-recorded the conversation, scheduled to last approximately 90 minutes, with the participant’s consent. A concept-elicitation approach was applied based on a semi-structured interview guide, which included open-ended questions to encourage spontaneous responses, and probes to obtain additional insights when deemed appropriate. Open-ended questions (eg, “How did endometriosis affect your life?”) were used to elicit the respondent’s experiences with endometriosis, referring to the time period prior to enrollment in the SPIRIT trials, and to encourage description of their symptoms and impacts on daily life in their own words. If not reported spontaneously, probing was used whereby women were requested to characterize endometriosis symptoms and their impacts in terms of frequency, duration, severity, and onset (where appropriate). Interviewers did not specifically probe whether pain symptoms occurred during menstrual or non-menstrual days for most concepts; however, spontaneously reported information related to the influence of menstruation on pain was captured.
Adverse Event Reporting
Women were asked to describe symptoms and impacts of endometriosis before participating in SPIRIT 1 or 2. If women spontaneously reported potential adverse events related to study drug experienced during SPIRIT 1 and 2 (including novel symptom or worsening of an existing symptom), these were reported in accordance with the clinical trial procedures (treatment-related adverse events are not presented here).
Data Analysis
Coding Scheme and Analysis Process
Interview audio recordings were anonymized and transcribed verbatim. Each transcript was considered a unit of analysis, and data from transcripts were aggregated. The initial coding scheme was developed based on the interview guide and research objectives, and it was updated to reflect terminology used by interviewed women and to incorporate emerging data. The coding scheme was applied and operationalized using the ATLAS.ti version 8.3.20 software (Atlas.ti GmbH, Berlin, Germany) for qualitative data analysis.
Coding was guided by established qualitative research methods including constant comparative method and grounded theory. Unique concepts were identified, and frequencies of concepts (both spontaneous and probed) were analyzed and reported with accompanying exemplary quotes.
Intercoder Reliability
Intercoder reliability (ICR), or the extent to which independent coders were concordant in coding, was evaluated using percentage agreement. Each of the three coders independently coded the first transcript, and percent agreement was derived by dividing the total number of concordant codes by the total number of codes used. Coders continued to evaluate ICR until a 90% agreement, determined a priori, was achieved. Although there is limited consensus for acceptable ICR threshold, 90% is considered acceptable and rigorous by the benchmarks (70–94%) available in the literature.13
Concept Saturation
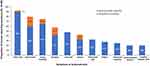
Concept saturation is achieved when additional interviews are unlikely to yield new information.14 Concepts spontaneously emerging from interviews were analyzed in cohorts (n = 10) based on collection order. In addition to evaluating saturation by comparing interview cohorts, graphs were developed to illustrate concept accumulation over the course of consecutive interviews (Figure 1).
 |
Figure 1 Saturation of spontaneously reported symptoms and impacts of endometriosis. Each cohort is represented by a colored marker: yellow represents the first 25% of patients (n=10, 25.0%), green represents the second 25% of patients (n=10, 25.0%), blue represents the third 25% of patients (n=10, 25.0%), and orange represents the last 25% of patients (n=10, 25.0%). Note: to journal: please could you move Figure 1 to where it is mentioned in the results section i.e. under the ‘ICR and Concept Saturation’ results section. The rationale for this is that the figure reports results from the analysis so is less appropriate in the methodology section |
Results
Participant Disposition and Demographics
Forty (SPIRIT 1, n = 13, 32.5%; SPIRIT 2, n = 27, 67.5%) English-speaking women across 25 US sites participated. Most women opted for phone (n = 35, 87.5%) versus web/internet-based video (n = 5, 12.5%) interviews. Women in this study had similar baseline characteristics to the overall SPIRIT 1 and 2 population, except for race, whereby a higher proportion of Black/African American women were included in the interview study. The average age of participants was 33 years, 60% (n = 24) were White, and the majority (>90%) self-reported some college or higher education level (Table 1).
 |
Table 1 Baseline Demographics, Educational Information, and Clinical Characteristics of Women with Endometriosis Intervieweda |
ICR and Concept Saturation
Acceptable ICR (ie, 90% agreement) was reached after coding the third transcript. No new concepts were spontaneously reported by women in the final interview cohort (n = 10), demonstrating adequacy of the sample size. Concept saturation was achieved for the spontaneously reported symptoms and impacts after the 13th (32.5%) and 17th (42.5%) interview, respectively (Figure 1).
Burden of Endometriosis: Symptoms
In total, 18 unique symptoms of endometriosis emerged from interviews, reported both spontaneously and on probing (ie, only following explicit probing from the interviewer), describing experiences of endometriosis prior to enrollment in the SPIRIT studies. Figure 2 shows the 10 most commonly reported endometriosis symptoms; Table 2 highlights example quotes from interviewees relating to these symptoms.
 |
Table 2 Quotes on Symptoms of Endometriosis Commonly Reported (≥20%) by Interviewed Women (Spontaneous and Probed Reporting Combined) |
More than 90% of women (n = 37) experienced pelvic pain, which was described as “pain [that] is comparable to labor pains”, “like my insides were ripping themselves apart”, or “like extreme cramps … like a sharp, shooting pain”. Dyspareunia was reported by 80.0% (n = 32) of women and reported as “excruciating … like being stabbed all the time” and “extremely painful” as it relates to sexual intercourse. All women with dyspareunia indicated that it had a negative impact on their sex lives. Heavy bleeding (referring to volume of bleeding; n = 30, 75%) was characterized as “bleed[ing] like a river” or “just too much blood. … I thought I was going to bleed to death sometimes”. When discussing heavy bleeding, women mentioned the need to frequently change menstrual hygiene products (eg, tampons, pads), as well as soiling clothes and linens. Women with bloating (n = 23, 57.5%) described its severity and how it affected their appearance with statements such as: “I look five months pregnant” or “My stomach… It still swells and gets puffy…”. Most women referred to bloating as a sensation (ie, a feeling of fullness) and a change in appearance (ie, visible distension) occurring due to endometriosis.
Symptoms reported by less than 50% of women included back pain (n = 19, 47.5%), described as “sharp knives or thorns” and “the pain will radiate down … my lower back”. Some women (n = 17, 42.5%) experienced nausea due to endometriosis-related pain, with one woman saying, “You’re so nauseous, and pain-wise, you just … don’t want to do anything. You don’t want to eat anything. You don’t even want to think about food.”
Abdominal pain was reported by almost a third of interviewed women (n = 13, 32.5%), and fatigue by 11 (27.5%). A quarter of respondents (n = 10, 25.0%) experienced headaches/migraines that they attributed to endometriosis, while eight women (20.0%) mentioned endometriosis-associated gastrointestinal distress, referring to it as “cramps, constipation, diarrhea, all of that mixed into one”. Additionally, lengthy/irregular cycles (referring to unpredictability and/or duration) attributed to endometriosis were reported by eight women (20.0%), one of whom said, “I was always bleeding all the time, like I had no specific date [for my period]” (Figure 2 and Table 2).
Less commonly (<20%) reported symptoms and signs included anemia, cramping (only captured when women indicated “cramping” as a unique sensation separate from pelvic and/or abdominal pain), and leg pain (12.5% of women experienced each of these symptoms). Cysts, vaginal pain, acne, and body temperature changes were mentioned by ≤10% of women.
Pain and Menstrual Status
Although most interviewed women indicated that pain occurred during both menstrual and non-menstrual days (n = 25 of 37, 67.6%), some reported pain only during menstrual days (n = 5 of 37, 13.5%) or only non-menstrual days (n = 4 of 37, 10.8%), while others did not make any specific distinction (n = 3 of 37, 8.1%) (Figure 3). There were no clear differences in descriptions of pelvic pain experienced during dysmenorrhea compared with NMPP; however, several women indicated that pain intensified during menstruation. Other types of pain (ie, back pain, abdominal pain, headaches/migraine) were more frequently reported during menstrual days only or during both menstrual and non-menstrual days (Figure 3).
 |
Figure 3 Pain concepts and their relationship to menstruation as reported by interviewed women with endometriosis (N=40). |
Impact of Endometriosis Symptoms
Thirty-three unique impacts of endometriosis symptoms were reported across 11 conceptual categories: physical, activities of daily living, social, sleep, emotional, appearance, financial, sex-related, work/school-related, fertility, and cognitive. The most common impacts of endometriosis are shown in Figure 4; example quotes from interviewees related to these impacts are provided in Table 3.
 |
Table 3 Example Quotes on Impacts of Endometriosis Reported, Both Spontaneously and on Probing, by ≥20% of Interviewed Women |
 |
Figure 4 Impacts of endometriosis symptoms commonly (≥20%) reported spontaneously and on probing by interviewed women. |
Impacts of endometriosis symptoms on physical functioning were experienced by >70% of women, of which needing to lie down (97.5%) and difficulty standing (92.5%) were the most prevalent ones.
Impacts on activities of daily living were frequently reported (Figure 4); 95% of women described that endometriosis symptoms made it difficult to exercise or complete leisure activities (eg, bicycle riding, running, attending concerts/movies), made them unable to do jobs around the house (eg, wash dishes, clean floors, do laundry), or unable to do the things they wanted (eg, attend birthday parties, vacations, other leisure activities).
With regard to social impacts, 92.5% of respondents mentioned that they were unable to attend social events or had cancelled preexisting plans due to endometriosis symptoms. Furthermore, endometriosis symptoms had a negative impact on relationships (n = 18, 45.0%), which one patient described as “I stopped being social, because I didn’t think people could understand what I was [experiencing].”
Nearly all women reported difficulties with sleeping (n = 36, 90.0%) due to endometriosis symptoms, of which >80% described impairments in sleep as repeatedly waking up during the night (n = 30 of 36, 83.3%); one woman mentioned “…waking up in the middle of the night with the pain and it hurting so bad that, no matter what position.”
Impacts on emotional well-being were also described, where women commonly expressed feeling like they could not cope with the signs/symptoms of endometriosis (n = 32; 80%).
More than 60% (n = 25, 62.5%) reported that appearance was negatively impacted as a result of endometriosis symptoms; common descriptions included appearing bloated, experiencing weight gain, and having bruxism as a response to endometriosis pain.
A negative impact of endometriosis symptoms on their finances was experienced by more than half of women (n = 24, 60.0%), mainly as a result of large medical bills due to frequent visits to healthcare personnel and/or surgical expenses (n = 9/24; 37.5%). Several women (n = 9/24; 37.5%) also noted that they lost wages due to their endometriosis.
Women felt that endometriosis symptoms had a negative impact on romantic relationships (n = 24, 60.0%), including their ability to have sex (n = 17, 42.5%).
Approximately half of women (n = 22, 55.0%) highlighted that endometriosis symptoms caused them to miss work or school (ie, not attending work/school, arriving late, or leaving early from scheduled work or coursework); one woman commented, “there would be times where I’ve had to leave work because of the pain”. Similarly, loss of productivity at work/school was highlighted by 21 women (52.5%), and a small proportion were unable to attend work or school for an extended period of time (ie, several months or years) due to endometriosis symptoms (n = 4, 10.0%).
Seven women (17.5%) mentioned that endometriosis impacted their ability to conceive.
Discussion
This study used a concept-elicitation approach with open-ended interview questions, allowing women to identify and describe endometriosis symptoms and impacts on daily life in their own words. Pelvic pain, dyspareunia, and heavy bleeding were the most commonly reported symptoms by respondents. Interviewees subsequently described how endometriosis symptoms impacted their physical functioning, activities of daily living, ability to participate in social activities and sleep, as well as the impact on their emotions, appearance, finances, sex life, work or school commitments, and fertility. Although interviewers did not specifically probe on pain in relation to menstruation, >60% of women spontaneously reported that pain occurred during both menstrual and non-menstrual days.
Results from this study confirm findings from previous studies evaluating endometriosis symptoms and their impacts. Prior qualitative research studies using concept-elicitation interviews in the US and Europe reported the most prevalent endometriosis symptoms as pelvic pain (or cramps), vaginal bleeding, dyspareunia, dysmenorrhea, and NMPP.9,15,16 Other endometriosis symptoms identified in the present study, such as bloating, back pain, nausea, abdominal pain, fatigue, headaches, gastrointestinal distress, and lengthy/irregular cycles, are concordant with endometriosis symptoms reported in the literature.9,15–18
Endometriosis burden arises not only from symptoms of the disease (eg pain) but also accumulatively from the consequences of these symptoms. The impact of endometriosis symptoms on women’s lives as reported in the present study were generally consistent with impacts reported in other qualitative research studies, and included impacts on daily activities, appearance, emotional functioning, financial impact, physical activity, sex-related impacts, sleep, social activities, and work/school-related impacts.8,9,15,19,20 A prior study focusing on endometriosis-related pain identified that pain symptoms were the main cause of impairments in physical activity, work and study, social and leisure activities, household activities, sleep, and sexual activity.16 In the present study, fertility was also identified as an impact; however, fertility reporting was subject to potential selection bias from the inclusion criteria of the SPIRIT trials, which specified that women were not to get pregnant over the study period. Overall, findings from the present analysis align with qualitative research studies published previously, adding to the body of evidence for endometriosis symptoms and their impacts.
The present study benefited from using open-ended questions and a concept-elicitation approach to allow for comprehensive data collection, whereby women could describe symptoms and impacts of endometriosis in their own words. Symptoms and impacts identified both spontaneously and on probing were considered; those reported spontaneously may represent the ones that are most bothersome or recognizable as being associated with endometriosis.9 The majority of endometriosis impacts were identified upon probing, which was most pronounced for impacts related to daily living activities, appearance, finance, and physical activity. The use of probing, in addition to spontaneous reporting, provides useful insights into the impact of endometriosis, and can help to identify impacts that are distal to the disease and may be less commonly discussed spontaneously with healthcare professionals in the clinical setting.
Potential limitations of this analysis include the lack of women with mild pain symptoms (due to SPIRIT study inclusion criteria) and restricting participation to English-speaking US women. Due to these limitations, findings may be less generalizable to the global population of women with endometriosis. Additionally, due to lack of probing on pain in relation to menstruation, some women may have reported pelvic pain in general, rather than specifying dysmenorrhea or NMPP. Furthermore, the heavy menstrual bleeding or abnormal bleeding reported in women with endometriosis may in part be attributable to adenomyosis, which is difficult to diagnose but also prevalent in this population.17,21–25 In SPIRIT 1 and 2, patients completed the Endometriosis Health Profile-30 (EHP-30) questionnaire to assess the effect of pain on normal daily activities;12 this may have led to interviewees mentioning some of the symptoms and impacts priorly assessed by the EHP-30 questionnaire. To minimize this effect, women were encouraged to spontaneously report symptoms and impacts important to their personal experience. Women were asked to report their endometriosis experience prior to enrollment in the SPIRIT trials; treatment response during the SPIRIT trials may have interfered with perceptions of endometriosis. Finally, women included in the present analysis were those who had moderate-to-severe dysmenorrhea and NMPP prior to entry of SPIRIT 1 and 2; thus, this population may have been more likely to report pain during both menstrual and non-menstrual days compared with women with endometriosis in general.
Conclusions
This interview study reports women’s personal experiences regarding the symptoms and impacts of endometriosis, as described in their own words. The most commonly reported symptoms of endometriosis were pelvic pain, dyspareunia, and heavy bleeding. Endometriosis symptoms were most frequently reported to impact physical activities, activities of daily living, social interaction, sleep, emotions, appearance, finances, sex life, work or school, and fertility. Importantly, these findings demonstrate the debilitating consequences of endometriosis symptoms, which limit and adversely impact women’s daily lives. The results reported here illustrate that patients consider the effect of endometriosis to be much broader than the common symptoms of dysmenorrhea, dyspareunia, and NMPP. This report can enable clinicians to better understand how women with endometriosis perceive their disease and may help providers identify important impacts of the disease that may not be readily discussed with patients.
Abbreviations
EHP-30, Endometriosis Health Profile-30; ICR, intercoder reliability; NMPP, non-menstrual pelvic pain.
Data Sharing Statement
Research data from the patient interviews that support the present analysis are not publicly available.
Acknowledgments
The authors thank AXON Communications (London, UK) for providing medical writing support, which was sponsored by Myovant Sciences GmbH, in collaboration with Pfizer, in accordance with Good Publication Practice guidelines. The authors also thank the patients that participated in the research and the other contributors to the research: Christopher Evans, Michelle Borges, Maggie Paulich, Elizabeth Hribal, and Kayla Scippa (Endpoint Outcomes, a Lumanity company, Boston, MA, USA). Martha Gauthier and Brooke Witherspoon are current employees of Endpoint Outcomes, a Lumanity company. Endpoint Outcomes was acquired by Lumanity in June 2022 and rebranded as Lumanity in September 2022.
Author Contributions
All authors made substantial contributions to the conception and design of the study, or acquisition of data, or analysis and interpretation of data, drafting the article or revising it critically for important intellectual content, and provided final approval of the version to be submitted.
Funding
This article was funded by Myovant Sciences GmbH, in collaboration with Pfizer, with research completed by Endpoint Outcomes (a Lumanity company) who were compensated by Myovant Sciences GmbH.
Disclosure
EH and VR are employed by Myovant Sciences and are shareholders of the company. MG and BW are employees of Endpoint Outcomes, a Lumanity company, which was compensated by Myovant Sciences to conduct this research. SKA has received grants from SOBI; personal fees for speaker bureau’s from AbbVie and is a consultant for Myovant. The authors report no other conflicts of interest in this work.
References
1. Acién P, Velasco I. Endometriosis: a disease that remains enigmatic. ISRN Obstet Gynecol. 2013;2013:242149. doi:10.1155/2013/242149
2. Rogers PA, D’Hooghe TM, Fazleabas A, et al. Priorities for endometriosis research: recommendations from an international consensus workshop. Reprod Sci. 2009;16:335–346. doi:10.1177/1933719108330568
3. Adamson GD, Kennedy S, Hummelshoj L. Creating solutions in endometriosis: global collaboration through the World Endometriosis Research Foundation. J Endometr. 2010;2:3–6. doi:10.1177/228402651000200102
4. Riazi H, Tehranian N, Ziaei S, et al. Clinical diagnosis of pelvic endometriosis: a scoping review. BMC Womens Health. 2015;15:39. doi:10.1186/s12905-015-0196-z
5. Hudson N. The missed disease? Endometriosis as an example of ‘undone science’. Reprod Biomed Soc Online. 2022;14:20–27. doi:10.1016/j.rbms.2021.07.003
6. Rogers PA, D’Hooghe TM, Fazleabas A, et al. Defining future directions for endometriosis research: workshop report from the 2011 World Congress of Endometriosis in Montpellier, France. Reprod Sci. 2013;20:483–499. doi:10.1177/1933719113477495
7. Christ JP, Yu O, Schulze-Rath R, et al. Incidence, prevalence, and trends in endometriosis diagnosis: a United States population-based study from 2006 to 2015. Am J Obstet Gynecol. 2021;225:500.e501–500.e509. doi:10.1016/j.ajog.2021.06.067
8. Nnoaham KE, Hummelshoj L, Webster P, et al. Impact of endometriosis on quality of life and work productivity: a multicenter study across ten countries. Fertil Steril. 2011;96:366–373.e368. doi:10.1016/j.fertnstert.2011.05.090
9. van Nooten FE, Cline J, Elash CA, Paty J, Reaney M. Development and content validation of a patient-reported endometriosis pain daily diary. Health Qual Life Outcomes. 2018;16:3. doi:10.1186/s12955-017-0819-1
10. Warzecha D, Szymusik I, Wielgos M, Pietrzak B. The impact of endometriosis on the quality of life and the incidence of depression-a cohort study. Int J Environ Res Public Health. 2020;17:3641. doi:10.3390/ijerph17103641
11. Parasar P, Ozcan P, Terry KL. Endometriosis: epidemiology, diagnosis and clinical management. Curr Obstet Gynecol Rep. 2017;6:34–41. doi:10.1007/s13669-017-0187-1
12. Giudice LC, As-Sanie S, Arjona Ferreira JC, et al. Once daily oral relugolix combination therapy versus placebo in patients with endometriosis-associated pain: two replicate phase 3, randomised, double-blind, studies (SPIRIT 1 and 2). Lancet. 2022;399:2267–2279. doi:10.1016/S0140-6736(22)00622-5
13. Campbell JL, Quincy C, Osserman J, Pedersen O. Coding in-depth semistructured interviews: problems of unitization and intercoder reliability and agreement. Sociol Methods Res. 2013;42:294–320. doi:10.1177/0049124113500475
14. Glaser BG, Strauss AL. The constant comparative method of qualitative analysis. In: The Discovery of Grounded Theory: Strategies for Qualitative Research. New York: Aldine de Gruyter; 1967.
15. Guan Y, Nguyen AM, Wratten S, et al. The endometriosis daily diary: qualitative research to explore the patient experience of endometriosis and inform the development of a patient-reported outcome (PRO) for endometriosis-related pain. J Patient Rep Outcomes. 2022;6:5. doi:10.1186/s41687-021-00409-8
16. Gater A, Taylor F, Seitz C, et al. Development and content validation of two new patient-reported outcome measures for endometriosis: the Endometriosis Symptom Diary (ESD) and Endometriosis Impact Scale (EIS). J Patient Rep Outcomes. 2020;4:13. doi:10.1186/s41687-020-0177-3
17. Zondervan KT, Becker CM, Missmer SA. Endometriosis. N Engl J Med. 2020;382:1244–1256. doi:10.1056/NEJMra1810764
18. Kalaitzopoulos DR, Samartzis N, Kolovos GN, et al. Treatment of endometriosis: a review with comparison of 8 guidelines. BMC Womens Health. 2021;21:397. doi:10.1186/s12905-021-01545-5
19. Moradi M, Parker M, Sneddon A, Lopez V, Ellwood D. Impact of endometriosis on women’s lives: a qualitative study. BMC Womens Health. 2014;14:123. doi:10.1186/1472-6874-14-123
20. Simoens S, Dunselman G, Dirksen C, et al. The burden of endometriosis: costs and quality of life of women with endometriosis and treated in referral centres. Hum Reprod. 2012;27:1292–1299. doi:10.1093/humrep/des073
21. Di Donato N, Montanari G, Benfenati A, et al. Prevalence of adenomyosis in women undergoing surgery for endometriosis. Eur J Obstet Gynecol Reprod Biol. 2014;181:289–293. doi:10.1016/j.ejogrb.2014.08.016
22. Zondervan KT, Becker CM, Koga K, et al. Endometriosis. Nat Rev Dis Primers. 2018;4:9. doi:10.1038/s41572-018-0008-5
23. Vannuccini S, Petraglia F. Recent advances in understanding and managing adenomyosis. F1000Res. 2019;8:238. doi:10.12688/f1000research.17242.1
24. Peric H, Fraser IS. The symptomatology of adenomyosis. Best Pract Res Clin Obstet Gynaecol. 2006;20:547–555. doi:10.1016/j.bpobgyn.2006.01.006
25. Chapron C, Vannuccini S, Santulli P, et al. Diagnosing adenomyosis: an integrated clinical and imaging approach. Hum Reprod Update. 2020;26:392–411. doi:10.1093/humupd/dmz049
[ad_2]
Source link