Columbia woman shares treatment journey during her battle with breast cancer

[ad_1]
COLUMBIA, Mo. (KMIZ)
It was a normal day at the gym for Columbia woman Leigh Ann Clayton when she noticed a couple of lumps around her armpit.
She was doing a pull-down exercise in October 2021 when she began to feel a stinging pain in her right armpit. She felt around and noticed the lumps.
She went to the doctor, who said there wasn’t a huge concern. But months went by, and the lumps didn’t go away.
She was diagnosed with Stage 3 triple-negative breast cancer in April 2022, when she was 47 years old.
“Hearing the diagnosis, the treatment, the side effects, you almost live like this out-of-body experience because you just cannot understand,” Clayton said. “It doesn’t make sense. I was scared.”
| Stage Zero | Non-invasive cancers inside the milk duct |
| Stage One | A small cancer that has not spread to the lymph nodes |
| Stage Two | Larger than stage one and has spread to a few lymph nodes |
| Stage Three | Larger tumors that are growing into nearby tissues and have already spread to nearby lymph nodes |
| Stage Four | Metastatic breast cancer, the cancer has spread beyond the breast and lymph nodes to other parts of the body. |
Chemotherapy infusions
Clayton received treatment at the Ellis Fischel Cancer Center. Her treatment journey started with nine months of chemotherapy infusions.
The American Cancer Society reports in triple-negative diagnoses, chemo is often given before surgery to shrink a large tumor and lymph nodes with cancer.
Dr. Debra Koivunen, medical director at the Ellis Fischel Breast Cancer Clinic, said chemotherapy infusions usually occur once every three weeks and are meant to stop cancer from spreading.
She said some women won’t be able to hold down a job while getting regular chemotherapy infusions, but others will only need to take a few days off after each treatment.
“I try to counsel my patients to not pick their therapy based on how much time they’re going to be off work, because in the long run, that’s a drop in the bucket,” Koivunen said. “We’re talking about the rest of their life, and we want them to pick the therapy that ultimately, 20 years down the road, they’re going to be glad that’s what they chose.”
Clayton was only about a year into her job at the University of Missouri Student Center and wanted to keep going to work throughout treatment. She would go in for chemo on Wednesdays and begin to feel the effects on Friday.
She said the fatigue was difficult.
“Those Sundays would come, and of course I’d be nauseous, no energy and not really wanting to do much,” Clayton said.

Clayton would have to take some days off here and there because of the chemo and said she leaned heavily on her family and friends. She said her coworkers and members of a Bible study group went with her to treatments and her family helped with chores around the house like taking care of her dog and mowing the lawn.
“You literally need help in every facet of life because you just really can’t get motivated to move,” Clayton said. “A lot of my family, a lot of my friends and of course my coworkers helped me through this treatment, and I couldn’t have gotten through it without them.”
Surgery
After months of chemotherapy, Clayton had a double mastectomy.
Koivunen said surgery is often the first step in the treatment process.
She said there are two options for surgery: a lumpectomy and a mastectomy. A lumpectomy saves the breast, as doctors will remove the cancer and some normal tissue. She quotes patients with between a 3% to 8% chance cancer could come back to the same breast at some point during their lifetime.
A mastectomy, on the other hand, removes the entire breast, leaving women with a flat chest and the option of reconstruction surgery or special-fitting bras. Koivunen said this surgery makes the chance of a tumor coming back less than 1%.
“If you’re worried about it coming back, that’s where the difference is between doing a lumpectomy and a mastectomy,” Koivunen said.
She said a lumpectomy is an outpatient procedure with most women recuperating in 7-10 days.
However, she said women who receive a mastectomy tend to spend the night in the hospital. She said if women get immediate reconstruction surgery that will add to their recovery time, estimating most women could be back to work within three to four weeks of the mastectomy.
“What we worry about with breast cancer is really not so much what’s in the breast — because I just told you how we can take care of that — we worry if it’s going to spread someplace else,” Koivunen said. “Because that is what’s going to shorten a lady’s life.”
Radiation therapy
Next for Clayton was five weeks of radiation therapy. According to the American Cancer Society, radiation uses high-energy rays to destroy cancer cells.
Koivunen said radiation treatment is every day, five days a week.
After radiation, Clayton was declared to be cancer free.
Immunotherapy
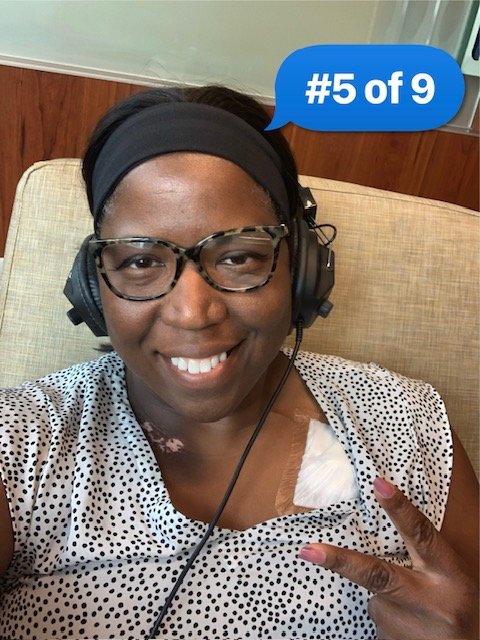
Clayton then went through nine treatments of immunotherapy infusions.
The American Cancer Society said this type of therapy is performed by using medicine to boost a patient’s immune system to recognize and destroy cancer cells.
Chemotherapy pill
Now, Clayton is taking a chemotherapy pill for one year.
She has 10 more months of taking the pill every day. She said she’s been told the first year after being cancer-free is a year that it could come back, so she is hoping that after these next 10 months will be free and clear.
“Once I get to that year, I think I’ll start to feel a little bit better,” Clayton said. “Every itch, sore or bump that I feel, I feel like, is this another round of cancer? I’m not as scared, but the fear is still real.”
Cost of treatment
The National Cancer Institute reports breast cancer is the most expensive form of cancer to treat, costing $29.8 billion nationwide in 2020.
Clayton said she has paid about $10,000 for treatment between 2022-2023, with more out-of-pocket costs on the way for reconstruction surgery.
“The first year, it was a little nerve-racking, because I hadn’t planned it. I didn’t budget for medications and hospital visits,” Clayton said. “So, it was a little tough the first year, but I managed.”
She said while the price tag was no easy pill to swallow, she was able to plan things out and feel better about the costs.
Advice for other patients
Clayton tells women to advocate for themselves.
Clayton initially went to the doctor when she first noticed the lumps in October 2021, but wasn’t diagnosed until she made another visit in 2022. She said many women, especially women of color, need to advocate for themselves.
The American Cancer Society reports Black women have the highest death rate from breast cancer, with 1-in-5 getting triple-negative breast cancer, like Clayton. Black women also have a higher chance of developing breast cancer before the age of 40, and have a younger median diagnosis age at 60 years old.
“It’s easy to go to the doctor and say, ‘I have an itch or something,’ but if you really feel like something’s wrong, you definitely need to advocate for yourself,” Clayton said.
Clayton said doctors already had a treatment plan for her triple-negative diagnosis, but Koivunen said breast cancer treatment is now more personalized for the patient. She tells patients there is time to do research, talk things over with family and fully understand the disease process before making any decisions.
“We’re personalizing the care of breast cancer much more now than we used to,” Koivunen said. “Taking into account what she wants to do, what kind of tumor she has, and how that tumor is slated to behave based on genomic testing.”
Clayton also said to let people help. Along with this, she said patients should take people with them to appointments to help them understand all of the information being given.
[ad_2]
Source link
