Overdose death rates increased significantly for Black, American Indian/Alaska Native people in 2020 | CDC Online Newsroom

[ad_1]
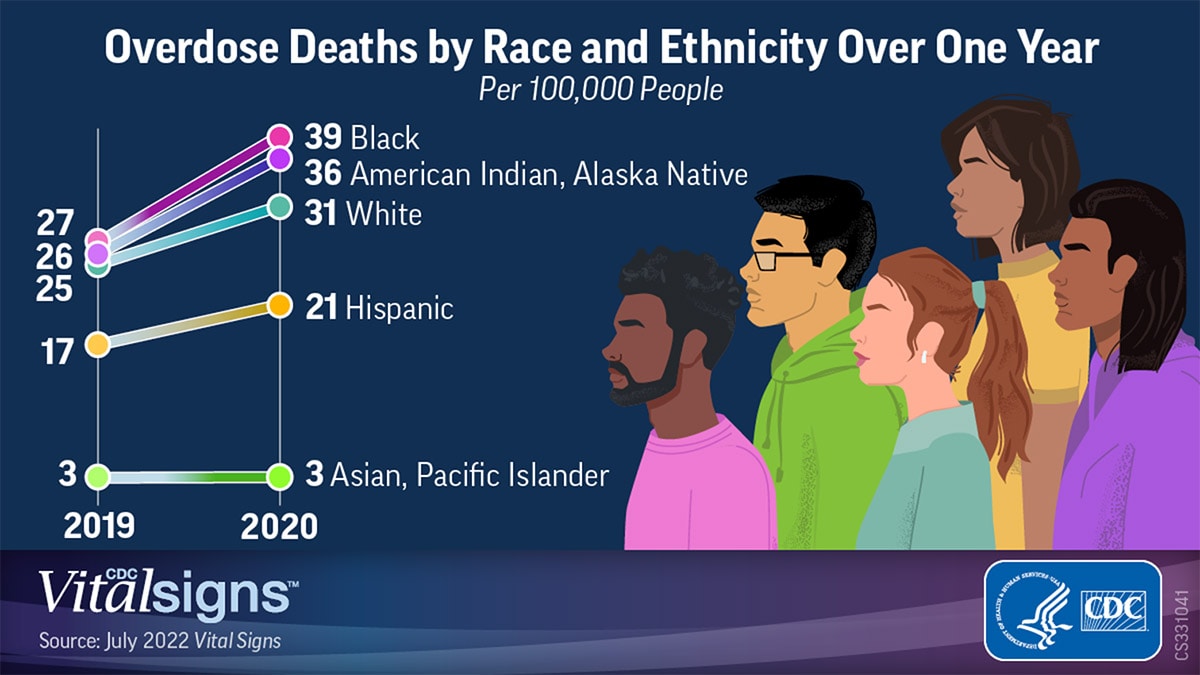
In 2020, overdose death rates (number of drug overdose deaths per 100,000 people) increased 44 percent for Black* people and 39 percent for American Indian and Alaska Native (AI/AN) people compared with 2019, according to a new CDC Vital Signs report with drug overdose data from 25 states and the District of Columbia. Overdose death rates in other groups, specifically White people, for whom the increase was 22 percent, are also at historic highs. Against the backdrop of the COVID-19 pandemic, disruption in access to prevention, treatment, harm reduction, and recovery support services has likely contributed to this growth in overdose deaths. Recent increases in deaths were largely driven by illicitly manufactured fentanyl and fentanyl analogs (IMFs).
Among the key findings for drug overdose deaths:
- In 2020, the overdose death rate among Black males 65 years and older was nearly seven times that of White males 65 years and older.
- Black people 15–24 years old experienced the largest rate increase (86 percent) compared with changes seen in other age/race groups during 2019–2020.
- Overdose death rates for AI/AN women 25–44 years of age were nearly two times that of White women 25–44 years of age.
Additionally the report analyzed drug overdose death rates by treatment access and income inequality, which continue to show concerning trends and widening disparities between different population groups:
- A history of substance use was common, but a history of receiving substance use treatment was not. Only about 1 in every 10 AI/AN and Hispanic people had reportedly received substance use treatment; evidence of treatment was even lower for Black people (1 in every 12).
- Opioid overdose rates in 2020 were higher in areas with higher availability of opioid treatment programs compared with areas with lower treatment availability, particularly among Black (34 vs. 17) and AI/AN (33 vs. 16) people per 100,000. Higher availability of treatment services does not mean improved access to care. The known differences in access, barriers to care, and healthcare mistrust could play a role in exacerbating inequities even when treatment is available in the community.
- In counties with more income inequality, there were greater disparities in overdose deaths, particularly among Black people, where the rate was more than two times as high in areas with more income inequality versus those with less income inequality.
- In counties with lowest income inequality, rates were highest among AI/AN people.
“The increase in overdose deaths and widening disparities are alarming,” said CDC Acting Principal Deputy Director Dr. Debra Houry, M.D., M.P.H. “Overdose deaths are preventable, and we must redouble our efforts to make overdose prevention a priority. We will continue to support and work collaboratively with communities like we do with CDC’s Overdose Data to Action (OD2A). Providing tailored tools and resources to combat overdose and address underlying risk factors will ultimately help reduce health disparities and save lives.”
Drug overdoses are preventable. The growing overdose crisis, particularly among people from racial and ethnic minority groups, requires prevention, treatment, recovery, and harm reduction efforts that are tailored to promote optimal health for all. Public health professionals, healthcare providers, policy makers, and communities can all play a role in preventing overdose deaths.
Three things we can do to prevent overdose deaths:
- Increase access and reduce barriers to proven treatment and recovery support services for all people who have substance use disorder(s) and, when appropriate, include culturally tailored practices.
- Raise awareness about illegally manufactured fentanyl and polysubstance use (the use of more than one drug) and reduce stigma around treatment, recovery, and harm reduction.
- Support harm reduction by expanding the distribution of and education about the life-saving overdose reversal drug, naloxone, expand access to harm reduction services (i.e., distribution of naloxone, fentanyl test strips, and syringe service programs), and expand education about substance use risks in populations that have been disproportionately impacted.
Find Treatment for Substance Use Disorder, including Opioid Use Disorder
If you or someone close to you needs help for a substance use disorder, talk to your doctor or call SAMHSA’s National Helpline at 1-800-662-HELP or go to SAMHSA’s Behavioral Health Treatment Services
Additional Resources:
If you have questions about any medicines, call the U.S. Department of Health and Human Services Poison Help Hotline at 1-800-222-1222.
988: The New 3-Digit Number Suicide and Crisis Lifeline
The National Suicide Prevention Lifeline has transitioned to (988) an easy-to-remember, three-digit dialing code that provides free and confidential emotional support to people in suicidal crisis or emotional distress 24 hours a day, 7 days a week, across the United States. The Lifeline comprises a national network of over 200 local crisis centers, combining custom local care and resources with national standards and best practices.
*Asian/Pacific Islander, American Indian/Alaska Native, Black, and White persons are non-Hispanic; Hispanic persons could be of any race.
For more information about this report, go to www.cdc.gov/vitalsigns.
[ad_2]
Source link