Racial disparities and prevalence of cardiovascular disease risk factors, cardiometabolic risk factors, and cardiovascular health metrics among US adults: NHANES 2011–2018

[ad_1]
Study design and study population
NHANES is an ongoing, cross-sectional survey that monitors the health and nutritional status of the US civilian, noninstitutionalized population. The sample selection entails using a complex, stratified, multistage probability design15, with written and informed consent obtained from each participant. The National Center for Health Statistics Research Ethics Review Board approved the NHANES study protocol16. The researcher’s Institutional Review Board (IRB) determined this secondary data analysis was exempt from review. All methods were performed in accordance with relevant guidelines and regulations and followed the Strengthening the Reporting of Observational Studies for Epidemiology (STROBE) guidelines for cross-sectional studies17.
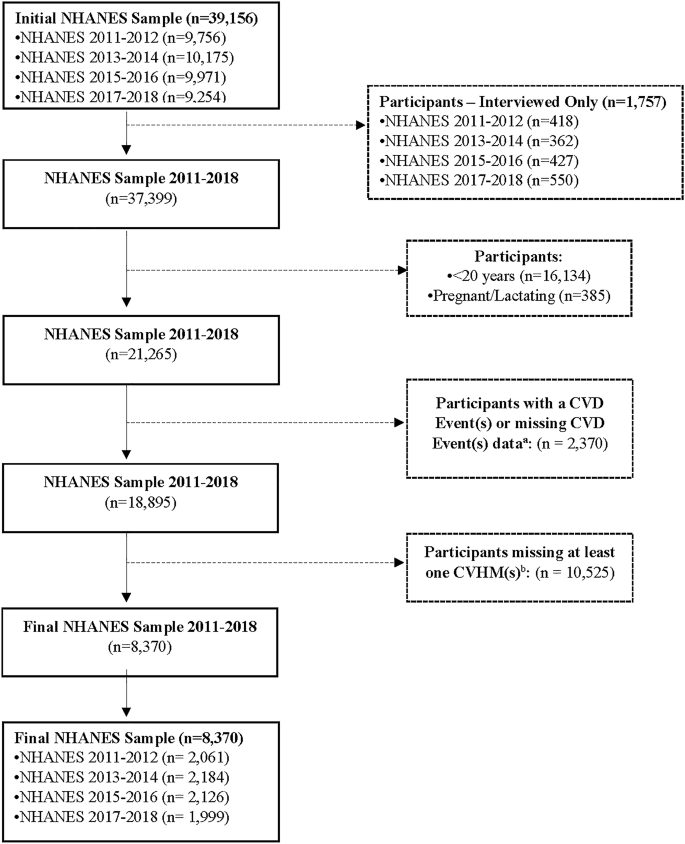
This analysis used data from the 2011 to 2018 NHANES (n = 39,156 participants). The analysis sample included non-pregnant, non-lactating adults 20 years and older who had measures for CVD and cardiometabolic risk factors and were free of coronary heart disease/heart failure, angina/angina pectoris, heart attack, and stroke (n = 18,895). We excluded participants who had incomplete information from the seven cardiovascular health metrics (CVHMs), yielding a final analysis sample size of 8370 participants (Fig. 1).
Flow chart of participant selection. NHANES National Health and Nutrition Examination Survey, CVD cardiovascular disease, CHF coronary heart failure, CHD coronary heart disease, ANG angina/angina pectoris, HAT heart attack, CVHM cardiovascular health metric, PA physical activity, SS smoke status, BMI body mass index, BP blood pressure, CHOL total cholesterol, FPG fasting plasma glucose. aCVD events includes CHF, CHD, ANG, HAT, Stroke. bCVHM includes PA, SS, BMI, BP, CHOL, FPG.
Demographic characteristics
We analyzed demographic information from the NHANES participants’ home interviews, including age, gender, race and ethnicity, education level, health insurance, current smoking status, and the poverty income ratio (PIR). We categorized the demographics as follows: age (20–39 years, 40–59 years, and ≥ 60 years); race and ethnicity (self-reported) non-Hispanic white, non-Hispanic black, Mexican American, other Hispanic, and non-Hispanic Asian; education (< 9th grade, 9th to 12th grade [but no high school diploma (HSD)], HSD or general education degree [GED], some college or associate degree, and ≥ bachelor’s degree); PIR, calculated by dividing the individual or family income by the US poverty guidelines specific to the survey year, and categorized as low income (PIR < 1.3), middle income (PIR 1.3 to < 3.5), and high income (PIR > 3.5)18. In addition, we included self-reported medication use for high blood pressure, diabetes, and high cholesterol.
Measurement of risk factors and cardiovascular health metrics
We used the mean of all provided systolic blood pressure (SBP) and diastolic blood pressure (DBP) measurements using the standard NHANES protocol19. Trained personnel in the NHANES mobile examination center followed standards to obtain weight and height and calculated body mass index (BMI), weight in kilograms/height in meters219. Smoking status was assessed from NHANES participants’ responses to the two variables, SMQ020 (smoked at least 100 cigarettes in life) and SMQ040 (do you now smoke cigarettes), categorized as current, former, and never smokers19. Laboratory values were collected using standard NHANES protocols19. We used non-fasted participants’ total cholesterol, high-density lipoprotein cholesterol (HDL-C), high-sensitivity C-reactive protein (hsCRP), fasted participants’ triglycerides, fasting blood glucose, and insulin. Homeostatic Model Assessment-Insulin Resistance (HOMA-IR) was calculated as fasting glucose (mg/dL) × fasting insulin (mU/L/405)20.
The Healthy Eating Index-2015 (HEI-2015) measures diet quality based on the 2015–2020 Dietary Guidelines for Americans21. The HEI-2015 includes 13 components, nine focusing on nutrient adequacy (e.g., total fruit, whole grains, and dairy) and four focusing on moderation (e.g., sodium and saturated fats). Each component has a designated maximum score of 5 or 10 points, which are summed for a maximum score of 100 points, indicating perfect adherence to the Dietary Guidelines for Americans 2015–2020. NHANES assesses physical activity using participants’ questionnaire responses regarding the frequency and duration of moderate to vigorous work and recreational activities19.
Cardiovascular disease risk factors
We included five CVD risk factors in our analysis: hypertension, hypercholesterolemia, obesity, diabetes, and smoking. We defined the CVD risk factors as the following (dichotomous variables [1 = present, 0 = absent]): hypertension, as mean SBP ≥ 130 mmHg, mean DBP ≥ 80 mmHg, or antihypertensive medication use22; hypercholesterolemia, as total cholesterol ≥ 240 mg/dL, or lipid-lowering medication use; obesity, BMI ≥ 30 kg/m2; and diabetes, as a fasting plasma glucose as ≥ 126 mg/dL, hemoglobin A1c (HbA1c) ≥ 6.5%, or hypoglycemic medication use. We classified participants as current or non-smokers. Each CVD risk factor was assigned a score of 1, indicating the participant had the CVD risk factor. We then summed the number of CVD risk factors for each participant, ranging from 0 to 5.
Cardiometabolic risk factors
We included five cardiometabolic risk factors in the analysis: low HDL-C, elevated triglycerides, glucose, HOMA-IR, and hsCRP. We defined the cardiometabolic risk factors as the following (dichotomous variables [1 = present, 0 = absent]): HDL-C < 40 mg/dL (men) and < 50 mg/dL (women) [in the context of metabolic syndrome, low HDL-C cut points differ for men and women; we elected not to use the low HDL-C cut point of < 40 mg/dL for both men and women]23; triglycerides ≥ 150 mg/dL; fasting plasma glucose ≥ 100 mg/dL or hypoglycemic medication use; HOMA-IR ≥ 2.520; and hsCRP > 3.0 mg/L24. Each cardiometabolic risk factor was assigned a score of 1. A score of 1 indicated the person had a cardiometabolic risk factor. We then summed the number of cardiometabolic risk factors (low HDL-C, elevated triglycerides, and glucose) for each participant, ranging from 0 to 3. We omitted HOMA-IR and hsCRP in the summation of the cardiometabolic risk factors because the data were not available for NHANES survey cycles 2011–2015.
Cardiovascular health metrics
The AHA defined seven CVHMs, behavior (diet, physical activity, smoking status, BMI) and health factors (blood pressure, total cholesterol, and fasting plasma glucose) (Table 1)13. The levels for each metric include poor (a score of 0), intermediate (a score of 1), or ideal (a score of 2). We scored CVHMs for each health behavior and factor (CVHM): 0 points (poor), 1 point (intermediate), or 2 points (ideal)25. We then summed each participant’s CVHM, creating a cardiovascular health (CVH) composite score ranging from 0 to 14 points, and then categorized participants into three CVH groups: poor (0–4 points), intermediate (5–9 points), and ideal (10–14 points)26.
Statistical analyses
All analyses were adjusted to account for the complex, multistage survey sampling design of the NHANES. We expressed data as mean (95% confidence interval). We calculated the age-adjusted prevalence of CVD and cardiometabolic risk factors and CVHMs for the total sample and each race and ethnic groups. We used the 2010 US Census population estimates for age-adjustment27; the proportion of adults aged 20–39 years, 40–59 years and ≥ 60 years was 36.7%, 37.9%, and 25.3%, respectively. We conducted pairwise comparisons of age-adjusted CVD and cardiometabolic risk factors, CVHMs, and CVH groups to determine which race and ethnic groups differed significantly. We used Bonferroni adjustment in the pairwise comparisons to account for multiple testing. Linear models were fit to estimate trends in the proportions or means of CVD and cardiometabolic risk factors and CVH metrics across survey cycles. All statistical tests were 2-sided, with a P-value of < 0.05 statistically significant. We conducted all analyses using SAS software, version 9.4 (SAS Institute, Cary, NC).
[ad_2]
Source link