State of Obesity 2022: Better Policies for a Healthier America

[ad_1]
(Washington, DC – September 27, 2022) – State of Obesity 2022: Better Policies for a Healthier America found that four in ten American adults have obesity, and obesity rates continue to climb nationwide and within population groups. These persistent increases in obesity rates underscore that obesity is caused by a combination of factors including societal, biological, genetic, and environmental, which are often beyond personal choice. The report’s authors conclude that addressing the obesity crisis will require attending to the economic and structural factors of where and how people live.
The report, based in part on 2021 data from the Centers for Disease Control and Prevention’s Behavioral Risk Factors Surveillance System, and analysis by TFAH, tracks rates of overweight and obesity by age, race, and state of residence.
Among the report’s findings are:
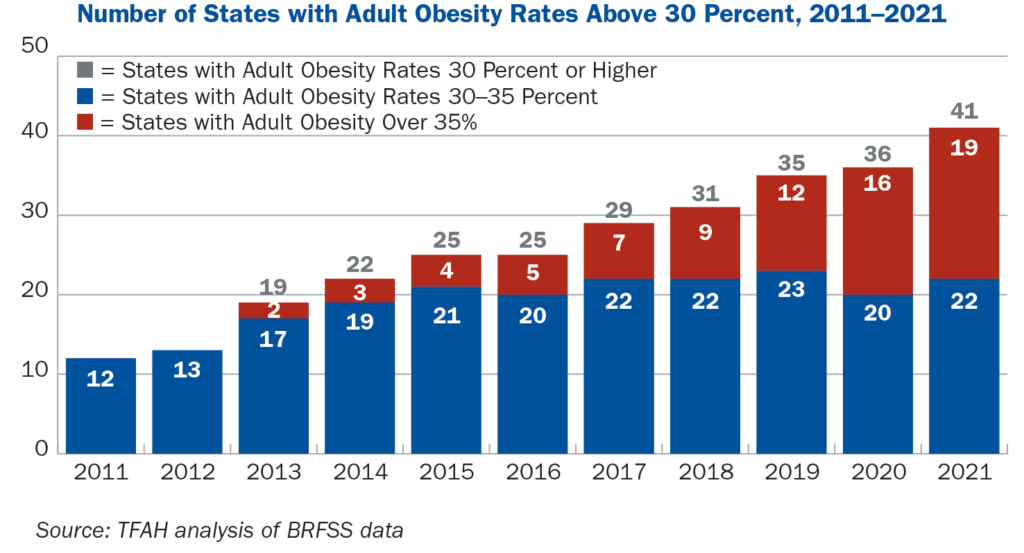
Nineteen states have adult obesity rates over 35 percent, up from 16 states last year. West Virginia, Kentucky, and Alabama have the highest rate of adult obesity at 40.6 percent, 40.3 percent, and 39.9 percent, respectively. The District of Columbia, Hawaii, and Colorado have the lowest adult obesity rates at 24.7 percent, 25 percent, and 25.1 percent respectively.
A decade ago, no state had an adult obesity rate at or above 35 percent.
National data from the 2017-2020 National Health and Nutrition Examination Survey also included in the report show the following:
- Nationally, 41.9 percent of adults have obesity.
- Black adults had the highest level of adult obesity at 49.9 percent.
- Hispanic adults had an obesity rate of 45.6 percent.
- White adults had an obesity rate of 41.4 percent.
- Asian adults had an obesity rate of 16.1 percent.
- Rural parts of the country had higher rates of obesity than did urban and suburban areas.
The report, released the day before the 2022 White House Conference on Hunger, Nutrition and Health, helps amplify the importance of focused attention on the obesity issue. Both the conference and the report spotlight the links between hunger, nutrition, and health, and diet-related diseases including obesity. In addition, they are intended to drive policy action to address food insecurity and health disparities, factors often at the root of diet-related health issues.
Obesity is multifactored and involves more than individual behavior
Structural and social determinants are significantly influencing the rates of obesity among adults and youth, according to the report authors. Factors such as structural racism, discrimination, poverty, food insecurity, housing instability, and lack of access to quality healthcare are key drivers of the differences in obesity rates across racial and ethnic groups. These systemic barriers make it inappropriate to assign blame to individuals with obesity for their weight. The purpose of this report is to analyze conditions in people’s lives which make them more likely to develop obesity and recommend policies to address those conditions.
A special section of the report looks at the relationship between food insecurity and obesity. Food insecurity, defined as being uncertain of having or unable to acquire enough food because of insufficient money or resources, is driven by many of the same social and economic factors that drive obesity including poverty and living in communities with many fast-food establishments but limited or no access to healthy, affordable foods such as available in full-service supermarkets. Being food and nutrition insecure often means families must eat food that costs less but is also high in calories and low in nutritional value.
Addressing obesity is critical because it is associated with a range of diseases including type 2 diabetes, heart disease, stroke, arthritis, sleep apnea, and some cancers. Obesity is estimated to increase U.S. healthcare spending by $170 billion annually (including billions by Medicare and Medicaid).
The report includes recommendations for policy actions that federal, state, and local policymakers and other stakeholders should take including:
- Increase funding for the CDC’s National Center for Chronic Disease Prevention and Health Programs to prevent obesity and related chronic diseases. Funding increases need to be sufficient to put proven obesity prevention programs to work in every state and should prioritize those communities where the need is greatest to address health inequities.
- Make healthy school meals for all students a permanent policy, extend COVID-19 flexibilities that expand nutrition access for students and their families, strengthen school nutrition standards, and increase students’ opportunities for physical activity during the school day.
- Expand the CDC’s social determinants of health program to address the upstream, structural drivers of chronic disease.
- Decrease food insecurity and improve the nutritional quality of available food by increasing funding for and participation in nutrition assistance programs such as the Supplemental Nutrition Assistance Program (SNAP), the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC), and the Child and Adult Care Food Program.
- End unhealthy food marketing to children by closing tax loopholes and eliminating business-cost deductions related to the advertising of unhealthy food and beverages to young people.
- Impose excise taxes on sugary drinks and devote the revenue to local obesity prevention programs and to reduce health disparities.
- Expand support for maternal and child health, including supporting breastfeeding.
- Fund active transportation projects like pedestrian and biking paths in all communities and make local spaces more conducive to physical activity.
- Expand access to healthcare and require insurance coverage with no cost sharing for U.S. Preventive Task Force recommended obesity prevention programs.
[ad_2]
Source link
